
- Altmetric
A 63-year-old woman presented with a painful lower leg lesion. Past medical history included hypertension, cerebrovascular disease, and previous cigarette smoking. Examination revealed a large nodular, necrotic ulcer, and livedo reticularis (Supplementary Figures S1 and S2). Initial investigations showed an elevated C-reactive protein level (60 mg/L; normal <5), eosinophilia (1.26 x 109/L; normal range: 0.04–0.4), and acute kidney injury with a serum creatinine level of 146 μmmol/L (normal range: 60–110), compared to 78 μmmol/L 2 months earlier. The urine protein:creatinine ratio was 146 mg/mmol (normal range: 0–30). Antineutrophil cytoplasm antibodies against myeloperoxidase were elevated (10 IU/ml; normal range: 0–5). The patient then developed painful cyanosis of her toes (Figure 1a) and a contrast-enhanced computed tomography scan showed diffuse, noncalcified atheromatous plaque in the thoracic aorta (Supplementary Figure S3, arrows). A renal biopsy showed focal ischemic glomerulosclerosis and mild tubulointerstitial inflammation. Necrotizing lesions, crescents, and arteritis were absent. A skin biopsy showed dermal arteriolar luminal occlusion with cholesterol clefts (Figure 1b, arrows) and associated endothelial-cell swelling with a reactive inflammatory infiltrate but no features of vasculitis or calciphylaxis. The myeloperoxidase antineutrophil cytoplasm antibody titre spontaneously fell to undetectable levels within 3 months of presentation. Despite supportive care, the patient’s kidney function deteriorated to require hemodialysis, and she died a year later. Cholesterol embolization follows fracturing of an atherosclerotic plaque and occurs most commonly following an invasive arterial procedure such as coronary angiography. In 1%–2% of patients, often those with severe atherosclerosis, it may be spontaneous. Cholesterol embolization may present with nonspecific features such as fever, weight loss, and elevated inflammatory markers, and so may mimic systemic autoimmune disease. The initial immune response is characterized by neutrophil infiltration of affected arterioles. Degranulation and release of cytoplasmic antigens by these activated neutrophils may generate antineutrophil cytoplasm antibodies. Diagnosis requires demonstration of cholesterol clefts in occluded blood vessels of affected organs. Treatment is mainly supportive.

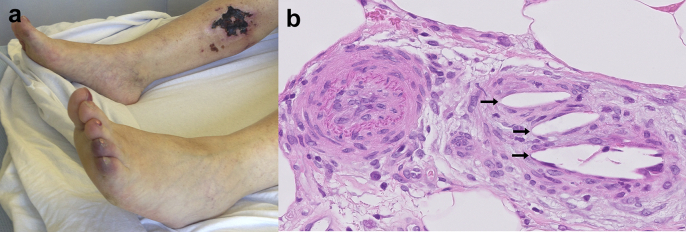
Skin necrosis, blue toe syndrome, and cholesterol embolization. (a) Necrotic ulcer on the upper part of the patient’s right shin and painful cyanosis of the right 4th and 5th toes in keeping with blue toe syndrome. (b) Skin biopsy with hematoxylin and eosin staining demonstrating dermal arteriolar occlusion with cholesterol clefts (arrows; original magnification ×40). To optimize viewing of this image, please see the online version of this article at www.kidney-international.org.
Figure S1.: Large nodular, necrotic ulcer on medial aspect on patient’s right shin.
Figure S2.: Livedo reticularis.
Figure S3.: Contrast-enhanced CT scan of thorax showing diffuse, noncalcified atheromatous plaque in the thoracic aorta (arrows).
 Antineutrophil cytoplasm antibody positivity, kidney impairment, and cholesterol embolization
Antineutrophil cytoplasm antibody positivity, kidney impairment, and cholesterol embolization