
Competing Interests: The authors have declared that no competing interests exist.
- Altmetric
Background and objectives
With the increase in the number of COVID-19 infections, the global health apparatus is facing insufficient resources. The main objective of the current study is to provide additional data regarding the clinical characteristics of the patients diagnosed with COVID-19, and in particular to analyze the factors associated with disease severity, lack of improvement, and mortality.
Methods
102 studies were included in the present meta-analysis, all of which were published before September 24, 2020. The studies were found by searching a number of databases, including Scopus, MEDLINE, Web of Science, and Embase. We performed a thorough search from early February until September 24. The selected papers were evaluated and analyzed using Stata software application version 14.
Results
Ultimately, 102 papers were selected for this meta- analysis, covering 121,437 infected patients. The mean age of the patients was 58.42 years. The results indicate a prevalence of 79.26% for fever (95% CI: 74.98–83.26; I2 = 97.35%), 60.70% for cough (95% CI: 56.91–64.43; I2 = 94.98%), 33.21% for fatigue or myalgia (95% CI: 28.86–37.70; I2 = 96.12%), 31.30% for dyspnea (95% CI: 26.14–36.69; I2 = 97.67%), and 10.65% for diarrhea (95% CI: 8.26–13.27; I2 = 94.20%). The prevalence for the most common comorbidities was 28.30% for hypertension (95% CI: 23.66–33.18; I2 = 99.58%), 14.29% for diabetes (95% CI: 11.88–16.87; I2 = 99.10%), 12.30% for cardiovascular diseases (95% CI: 9.59–15.27; I2 = 99.33%), and 5.19% for chronic kidney disease (95% CI: 3.95–6.58; I2 = 96.42%).
Conclusions
We evaluated the prevalence of some of the most important comorbidities in COVID-19 patients, indicating that some underlying disorders, including hypertension, diabetes, cardiovascular diseases, and chronic kidney disease, can be considered as risk factors for patients with COVID-19 infection. Furthermore, the results show that an elderly male with underlying diseases is more likely to have severe COVID-19.
Introduction
On December 31, 2019, a cluster of cases of pneumonia with an unknown source was reported in Wuhan, China, related to the Huanan seafood wholesale market [1, 2]. Subsequently, on January 9, 2020, the Chinese Center for Disease Control and Prevention announced its causative factor as the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This global disorder, caused by SARS-CoV-2, became known as COVID-19. Just two months later, on March 11, 2020, the Director General of the World Health Organization (WHO) designated the spread of COVID-19 as a pandemic [3, 4].
As of October 15, 2020, a total of 38,394,169 confirmed COVID-19 patients and 1,089,047 dead cases have been reported by WHO globally, and as of the time of this writing, the number of patients is increasing. In addition, 235 countries, regions, or territories with cases of COVID-19 infection have been identified worldwide [5]. The number of COVID-19 infected patients is increasing worldwide, and due to its correlation with a high morbidity and mortality rate, this trend has caused a new global phobia called Coro-phobia [6]. According to the results of a number of studies, COVID-19 infection can be diagnosed based on several symptoms, including cough, fever, fatigue, diarrhea, myalgia, and dyspnea [7–9].
Huang et al. evaluated the clinical features of 41 cases with COVID-19 infection, and their results showed that 13 (32%) cases had comorbidities, such as hypertension, chronic obstructive pulmonary disease, diabetes, and cardiovascular disease [10]. In addition, Guan et al. reported the results of 1,099 cases of COVID-19 infection, indicating that 261 (23.7%) cases had underlying diseases [11]. These studies and similar investigations show that some complications can be considered as risk factors for negative outcomes in patients with COVID-19 infection [12].
Furthermore, Lai et al. [13] realized that the mortality rate was associated with the country’s healthcare resources. However, in many countries, the intensive care units (ICUs) and the invasive ventilators are not enough to treat critically-infected patients. Consequently, clinical operators should consider the risk factors for critical cases of COVID-19, correctly assign medical resources, identify severe patients in the early stages of the disease, and devise an appropriate treatment plan to reduce the mortality rate and improve the effectiveness of the treatment [11]. Therefore, knowing the risk factors and the underlying diseases in COVID-19 patients is important for healthcare professionals, especially for immunocompromised people and the elderly. Subsequently, the evaluation of the prevalence of chronic diseases, such as hypertension, kidney disease, cardiovascular disease, and diabetes, is considered as one of the most important measures to reduce negative outcomes in COVID-19 patients [14].
Currently, we have no approved vaccines or curative drugs against the new COVID-19 infection; hence, to prevent COVID-19 infection, a systematic review and meta-analysis has been conducted to study the prevalence of common comorbidities by analyzing studies focusing on clinical risk factors for COVID-19.
Materials and methods
Study selection
We searched PubMed, Scopus, Web of Science, and Embase databases to identify relevant studies that were published on COVID-19 until September 24, 2020. The keywords for our search included: Kidney, COVID, Hypertension, Diabetes, ((Heart) OR Cardio-), and Comorbidities. Moreover, the citations in the identified studies were also scanned in order to identify references related to the subject matter.
Inclusion and exclusion criteria
All studies evaluating the clinical risk factors, underlying diseases, and comorbidities of COVID-19 have been reviewed. For our final analysis, the studies selected should report data on the prevalence of each of the risk factors for the severity of COVID-19 and its comorbidities in patients with COVID-19 infection, including hypertension, chronic kidney disease, diabetes, cardiovascular and cerebrovascular diseases, and coronary heart disease. Only human investigations were selected. The full texts of the relevant studies were assessed based on the inclusion and exclusion criteria. Studies that did not have adequate data, non-human studies, duplicate publications, and non-English publications (except for those with useful abstract data) were excluded.
Data extraction
All the selected papers were independently evaluated and screened by two authors (M.F. and K.V.), and any disagreements were resolved through discussion. The following data were collected for the final analysis: prevalence of hypertension, chronic kidney disease, diabetes, cardiovascular and cerebrovascular diseases, and coronary heart disease, along with the prevalence of symptoms such as fever, dyspnea, diarrhea, cough, fatigue, and myalgia.
Statistical analysis
Because the effect size in this study was based on proportion (i.e., prevalence of hypertension, chronic kidney disease, diabetes, cardiovascular and cerebrovascular diseases, and coronary heart disease), binomial distribution was employed to calculate the variance for each study. The prevalence in various studies were combined using the average weight. An inverse relationship between the variance of the study and its weight was observed. The I2 index was applied to evaluate the heterogeneity. In the case of heterogeneous studies, the random effects model were used. To analyze the data, Stata software application (version 14) was used. The Metaprop (meta-analysis for proportion) was used in Stata when p was close to 0 or 1. Moreover, to stabilize the variances, we used Freeman-Tukey Double Arcsine Transformation [15]. This study was performed with the approval of the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1399.084).
Publication bias
Publication bias was graphically defined by the Funnel plot. This funnel plot is a scatter plot with 2 variates (x, y) that evaluates the research estimate of the effect size against its sample size. A linear regression analysis was conducted for publication bias, which includes both slope and intercept parameters. It was calculated based on the following equation:
i = 1… r (r = the number of studies), yi = standardized estimate, xi = precision of studies, εi = error terms
Quality assessment
The Newcastle-Ottawa Scale (NOS) was employed to assess the quality of each included paper [16]. This scale includes 8 assessment items for evaluating the quality of studies, including ‘selection’, ‘comparability’, and ‘outcome’, based on the Ottawa checklist for the cross-sectional studies. Based on the score standard in NOS, cross-sectional studies can be classified as Very Good Studies (9–10 points), Good Studies (7–8 points), Satisfactory Studies (5–6 points), and Unsatisfactory Studies (0 to 4 points) (Table 1 in S1 File).
Results and discussion
Study selection
The current study was carried out based on the PRISMA checklist [17]. It should be noted that initially, 113 studies were identified through primary search on PubMed, 111 were identified by searching Scopus, 136 were identified by searching Embase, and 85 were identified by searching Web of Science. However, 284 of those 445 articles were excluded because of duplication. After screening the titles and abstracts of all identified papers, 22 more studies were excluded due to being review articles, case reports, and non-English articles, or due to unavailable abstracts. The full texts of the 139 remaining studies were reviewed, and 37 studies were excluded due to ineligible sample size (n = 12), lack of sufficient data (n = 21), or unavailable full text (n = 4). Finally, 102 articles, published from February, 2020 to July, 2020, were selected for the meta-analysis (Fig 1, Table 1).

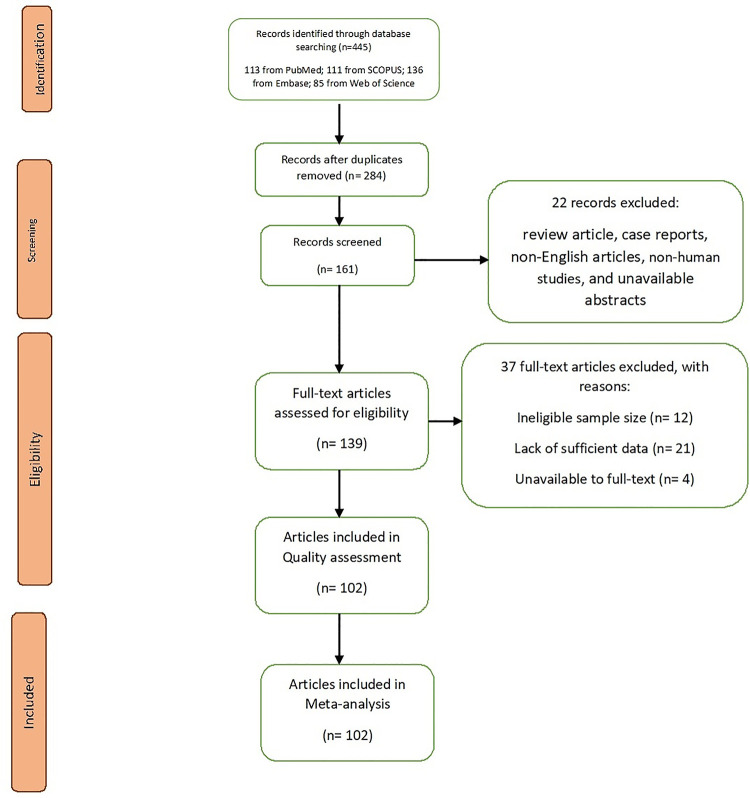
Study flow diagram.

| study | Place | Median age | Exposure history (No.) | Patients (No.) | Symptoms (No.) | Comorbidities (No.) | Mortality rate (%.) | Total Score | Total Quality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Male | Female | Fever | Cough | Fatigue or Myalgia | Diarrhea | Dyspnea | All | Hypertension | Diabetes | Cardiovascular disease | Chronic kidney disease | |||||||
| [18] | China | 56 | 73 | 191 | 119 | 72 | 180 | 151 | 44 | 9 | 56 | 91 | 58 | 36 | 2 | 28.27 | 10 | Very Good | |
| [19] | China | 3 | 85 | 62 | 23 | 78 | 19 | 50 | 16 | 50 | 58 | 32 | 19 | 3 | 8 | Good | |||
| [20] | China | 57.00 | 140 | 71 | 69 | 110 | 90 | 90 | 18 | 44 | 90 | 42 | 17 | 2 | 9 | Very Good | |||
| [21] | China | 59.00 | 174 | 76 | 98 | 136 | 56 | 47 | 21 | 42 | 43 | 37 | 32 | 13 | 9 | Very Good | |||
| [22] | China | 1590 | 904 | 674 | 1351 | 1052 | 584 | 57 | 331 | 399 | 269 | 130 | 59 | 269 | 3.10 | 8 | Good | ||
| [23] | China | 51.00 | 99 | 201 | 128 | 73 | 188 | 163 | 65 | 80 | 66 | 39 | 22 | 8 | 2 | 21.90 | 9 | Very Good | |
| [24] | China | 69.00 | 339 | 166 | 173 | 311 | 179 | 135 | 43 | 138 | 138 | 54 | 53 | 13 | 19.17 | 9 | Very Good | ||
| [25] | China | 73.00 | 25 | 10 | 15 | 23 | 25 | 16 | 10 | 8 | 5 | 100.00 | 5 | satisfactory | |||||
| [26] | U.S | 7162 | 2692 | 784 | 647 | 213 | 6 | satisfactory | |||||||||||
| [27] | U.S | 180 | 153 | 155 | 62 | 48 | 144 | 159 | 79 | 47 | 45 | 20 | 9 | Very Good | |||||
| [28] | China | 50.00 | 311 | 1012 | 524 | 488 | 761 | 531 | 170 | 152 | 231 | 114 | 46 | 27 | 15 | 9 | Very Good | ||
| [1] | China | 49.00 | 27 | 41 | 30 | 11 | 40 | 31 | 18 | 1 | 22 | 13 | 6 | 8 | 6 | 14.63 | 8 | Good | |
| [29] | China | 99 | 67 | 32 | 82 | 81 | 1 | 2 | 31 | 50 | 11.00 | 7 | Good | ||||||
| [12] | China | 56.00 | 12 | 138 | 75 | 63 | 136 | 82 | 96 | 14 | 43 | 64 | 43 | 14 | 20 | 4 | 4.30 | 9 | Very Good |
| [30] | China | 17 | 9 | 8 | 12 | 13 | 4 | 2 | 3 | 1 | 7 | Good | |||||||
| [11] | China | 47.00 | 1099 | 637 | 459 | 473 | 745 | 419 | 42 | 205 | 261 | 165 | 81 | 8 | 1.40 | 8 | Good | ||
| [31] | China | 41.00 | 23 | 62 | 35 | 27 | 48 | 50 | 32 | 3 | 20 | 5 | 1 | 1 | 0.00 | 6 | satisfactory | ||
| [32] | China | 0 | 80 | 39 | 41 | 63 | 30 | 18 | 1 | 30 | 38 | 1 | 0.00 | 7 | Good | ||||
| [33] | China | 57.00 | 0 | 137 | 61 | 76 | 112 | 66 | 44 | 11 | 26 | 27 | 13 | 14 | 10 | 11.68 | 8 | Good | |
| [34] | China | 40.00 | 61 | 31 | 30 | 60 | 39 | 35 | 6 | 3 | 12 | 5 | 1 | 0.00 | 9 | Very Good | |||
| [35] | China | 52 | 35 | 17 | 51 | 40 | 6 | 33 | 21 | 9 | 5 | 61.54 | 6 | satisfactory | |||||
| [36] | China | 187 | 91 | 96 | 61 | 28 | 6 | 23.00 | 9 | Very Good | |||||||||
| [37] | Italy | 355 | 72 | 100.00 | 7 | Good | |||||||||||||
| [38] | China | 12 | 8 | 4 | 10 | 11 | 4 | 2 | 3 | 2 | 4 | 2 | 6 | satisfactory | |||||
| [39] | China | 9 | 5 | 4 | 8 | 5 | 4 | 1 | 0 | 1 | 0 | 0 | 3 | Unsatisfactory | |||||
| [40] | China | 31974 | 44672 | 22981 | 21691 | 2683 | 1102 | 873 | 2.30 | 8 | Good | ||||||||
| [10] | China | 38.00 | 0 | 78 | 39 | 39 | 34 | 8 | 5 | 7 | Good | ||||||||
| [41] | China | 63.00 | 701 | 367 | 334 | 213 | 297 | 233 | 100 | 14 | 16.10 | 9 | Very Good | ||||||
| [42] | China | 57.00 | 193 | 95 | 98 | 171 | 134 | 75 | 35 | 70 | 105 | 66.32 | 10 | Very Good | |||||
| [43] | China | 62.00 | 274 | 171 | 103 | 249 | 185 | 137 | 77 | 120 | 133 | 93 | 47 | 23 | 4 | 41.24 | 9 | Very Good | |
| [44] | China | 72.50 | 82 | 54 | 28 | 64 | 53 | 38 | 10 | 52 | 62 | 46 | 15 | 17 | 8 | Good | |||
| [45] | China | 5 | 4 | 1 | 5 | 5 | 3 | 5 | 2 | 1 | 8 | Good | |||||||
| [46] | China | 64.00 | 416 | 205 | 211 | 334 | 144 | 55 | 16 | 117 | 127 | 60 | 10 | Very Good | |||||
| [47] | China | 54.00 | 116 | 67 | 49 | 43 | 18 | 5 | 9 | Very Good | |||||||||
| [48] | US | 21 | 11 | 11 | 17 | 18 | 7 | 10 | 52.40 | 7 | Good | ||||||||
| [49] | China | 54.00 | 203 | 108 | 95 | 181 | 122 | 16 | 10 | 3 | 88 | 43 | 16 | 16 | 8 | 12.80 | 9 | Very Good | |
| [50] | China | 50.00 | 91 | 37 | 54 | 65 | 55 | 40 | 21 | 3 | 15 | 8 | 0.00 | 6 | satisfactory | ||||
| [51] | China | 58.00 | 452 | 235 | 217 | 423 | 152 | 212 | 122 | 232 | 201 | 135 | 75 | 27 | 10 | 36.70 | 9 | Very Good | |
| [52] | China | 69 | 32 | 37 | 30 | 38 | 29 | 10 | 20 | 9 | 7 | 8 | 7.50 | 8 | Good | ||||
| [53] | China | 55.00 | 8 | 221 | 108 | 113 | 200 | 136 | 156 | 25 | 64 | 78 | 54 | 22 | 22 | 5.40 | 9 | Very Good | |
| [54] | China | 50.00 | 90 | 39 | 51 | 70 | 57 | 19 | 5 | 45 | 17 | 5 | 3 | 8 | Good | ||||
| [55] | China | 109 | 74 | 35 | 99 | 77 | 58 | 29 | 75 | 65 | 34 | 9 | Very Good | ||||||
| [56] | China | 54.00 | 47 | 102 | 53 | 49 | 83 | 50 | 56 | 11 | 35 | 47 | 28 | 11 | 5 | 4 | 16.70 | 9 | Very Good |
| [57] | Italy | 63.00 | 1591 | 1304 | 287 | 1043 | 509 | 180 | 223 | 36 | 9 | Very Good | |||||||
| [58] | US | 63.00 | 5700 | 3437 | 2263 | 5700 | 3026 | 1808 | 268 | 21.00 | 9 | Very Good | |||||||
| [59] | China | 68.00 | 54 | 24 | 13 | 48.10 | 6 | satisfactory | |||||||||||
| [60] | China | 200 | 99 | 101 | 161 | 101 | 137 | 16 | 17.00 | 10 | Very Good | ||||||||
| [61] | China | 64.91 | 47 | 26 | 21 | 12 | 18 | 5 | 6 | satisfactory | |||||||||
| [62] | China | 110 | 60 | 50 | 57 | 19 | 16 | 9 | 9 | Very Good | |||||||||
| [63] | China | 61.00 | 323 | 166 | 157 | 271 | 164 | 14 | 105 | 47 | 7 | 9 | Very Good | ||||||
| [64] | China | 49 | 31 | 18 | 39 | 17 | 9 | 4 | 6 | 16 | 6 | satisfactory | |||||||
| [65] | China | 47.00 | 298 | 149 | 149 | 192 | 54 | 6 | 6 | 38 | 19 | 11 | 8 | Good | |||||
| [66] | China | 265 | 220 | 131 | 67 | 17 | 5 | 52 | 21 | 14 | 9 | Very Good | |||||||
| [67] | China | 45.00 | 242 | 119 | 123 | 162 | 132 | 72 | 15 | 21 | 36 | 15 | 9 | 0.80 | 10 | Very Good | |||
| [68] | China | 48.00 | 84 | 48 | 36 | 54 | 43 | 16 | 6 | 3 | 12 | 10 | 5 | 8 | Good | ||||
| [69] | China | 55.00 | 109 | 59 | 50 | 90 | 67 | 62 | 12 | 37 | 12 | 7 | 10 | 28.40 | 9 | Very Good | |||
| [70] | China | 60.00 | 548 | 279 | 269 | 476 | 415 | 258 | 179 | 310 | 166 | 83 | 10 | 16.50 | 9 | Very Good | |||
| [71] | China | 52.00 | 113 | 66 | 47 | 91 | 26 | 9 | 1.80 | 9 | Very Good | ||||||||
| [72] | China | 60.00 | 27 | 12 | 15 | 21 | 16 | 3 | 11 | 13 | 5 | 6 | 3 | 37.00 | 8 | Good | |||
| [73] | China | 136 | 58 | 78 | 115 | 85 | 24 | 17 | 75 | 53 | 24 | 6 | 2 | 0.00 | 9 | Very Good | |||
| [73] | China | 652 | 349 | 303 | 521 | 421 | 115 | 20 | 143 | 73 | 33 | 5 | 5 | 0.00 | 9 | Very Good | |||
| [74] | Bolivia | 39.00 | 12 | 6 | 6 | 9 | 9 | 5 | 2 | 2 | 1 | 0.00 | 6 | Satisfactory | |||||
| [75] | China | 45.00 | 104 | 161 | 80 | 81 | 122 | 101 | 64 | 17 | 23 | 33 | 22 | 7 | 0.00 | 9 | Very Good | ||
| [76] | China | 47.00 | 113 | 135 | 72 | 63 | 120 | 102 | 44 | 18 | 18 | 43 | 13 | 12 | 7 | 0.70 | 9 | Very Good | |
| [77] | China | 37 | 14 | 23 | 15 | 12 | 0 | 10 | 8 | 4 | 0.00 | 6 | Satisfactory | ||||||
| [78] | China | 214 | 87 | 127 | 132 | 107 | 41 | 83 | 51 | 30 | 15 | 6 | 0.00 | 9 | Very Good | ||||
| [79] | China | 65.00 | 112 | 57 | 55 | 98 | 79 | 63 | 36 | 19 | 0.00 | 9 | Very Good | ||||||
| [80] | China | 136 | 90 | 46 | 52 | 71 | 66 | 27 | 102 | 41 | 27 | 3 | 0.00 | 8 | Good | ||||
| [81] | China | 70.00 | 25 | 19 | 6 | 16 | 12 | 6 | 8 | 100.00 | 8 | Good | |||||||
| [81] | China | 51.00 | 149 | 60 | 89 | 36 | 25 | 11 | 8 | 0.00 | 8 | Good | |||||||
| [82] | Singapore | 47.00 | 18 | 9 | 9 | 13 | 15 | 3 | 2 | 5 | 4 | 1 | 5 | unsatisfactory | |||||
| [83] | Korea | 75.50 | 54 | 33 | 21 | 49 | 16 | 32 | 5 | 100.00 | 7 | Good | |||||||
| [84] | China | 92 | 49 | 43 | 65 | 51 | 13 | 16 | 2 | 100.00 | 7 | Good | |||||||
| [85] | China | 168 | 86 | 82 | 156 | 121 | 65 | 44 | 59 | 57 | 41 | 20 | 9 | 2 | 10.10 | 10 | Very Good | ||
| [86] | China | 13 | 10 | 3 | 13 | 10 | 8 | 2 | 12 | 2 | 1 | 38.50 | 7 | Good | |||||
| [86] | China | 12 | 2 | 10 | 11 | 7 | 8 | 3 | 8 | 0 | 0 | 0.00 | 7 | Good | |||||
| [87] | UK | 82.00 | 101 | 64 | 37 | 9 | 4 | 9 | 3 | 67 | 54 | 36 | 18 | 21 | 74.20 | 8 | Good | ||
| [88] | China | 2 | 3 | 2 | 1 | 1 | 2 | 1 | 2 | 0 | 1 | 0 | 0.00 | 6 | satisfactory | ||||
| [89] | China | 134 | 149 | 81 | 68 | 114 | 87 | 11 | 2 | 52 | 28 | 0.00 | 7 | Good | |||||
| [90] | China | 31 | 81 | 42 | 39 | 59 | 48 | 7 | 3 | 34 | 21 | 12 | 10 | 8 | 3 | 4.00 | 8 | Good | |
| [91] | Korea | 77.00 | 66 | 37 | 29 | 61 | 30 | 23 | 10 | 5 | 9 | Very Good | |||||||
| [92] | China | 52.00 | 108 | 43 | 65 | 80 | 84 | 28 | 8 | 15 | 25 | 16 | 5 | 4 | 11.10 | 9 | Very Good | ||
| [93] | China | 53.00 | 425 | 476 | 271 | 205 | 390 | 269 | 109 | 205 | 113 | 49 | 38 | 4 | 8.00 | 9 | Very Good | ||
| [94] | China | 54.00 | 37 | 155 | 86 | 79 | 126 | 97 | 60 | 7 | 50 | 37 | 15 | 15 | 6 | 0.00 | 9 | Very Good | |
| [95] | China | 186 | 487 | 259 | 228 | 99 | 29 | 11 | 7 | 0.00 | 9 | Very Good | |||||||
| [96] | USA | 72 | 167 | 55 | 112 | 74 | 38 | 68 | 43 | 21 | 8 | Good | |||||||
| [97] | Italy | 65 | 410 | 229 | 111 | 203 | 69 | 47 | 10 | Very Good | |||||||||
| [98] | USA | 45 | 100 | 56 | 44 | 71 | 87 | 21 | 10 | 38 | 19 | 10 | 6 | 8 | Good | ||||
| [99] | Italy | 99 | 80 | 19 | 39 | 63 | 30 | 15 | 9 | Very Good | |||||||||
| [100] | USA | 69 | 105 | 53 | 52 | 49 | 76 | 51 | 24 | 56 | 62 | 35 | 40 | 27 | 33 | 9 | Very Good | ||
| [101] | Greece | 21 | 17 | 4 | 7 | 2 | 0 | 0 | 9 | Very Good | |||||||||
| [101] | Greece | 24 | 18 | 6 | 11 | 4 | 3 | 1 | 9 | Very Good | |||||||||
| [101] | Greece | 45 | 37 | 8 | 27 | 11 | 16 | 3 | 9 | Very Good | |||||||||
| [102] | Italy | 68 | 236 | 177 | 59 | 230 | 144 | 83 | 37 | 127 | 15 | 10 | Very Good | ||||||
| [103] | USA | 52.7 | 13442 | 7841 | 5957 | 3043 | 2710 | 2086 | 809 | 9 | Very Good | ||||||||
| [104] | China | 83 | 44 | 39 | 72 | 65 | 15 | 7 | 9 | 15 | 5 | 7 | 1 | 8 | Good | ||||
| [105] | China | 296 | 140 | 156 | 213 | 197 | 42 | 30 | 6.4 | 9 | Very Good | ||||||||
| [106] | China | 1590 | 904 | 674 | 1351 | 1052 | 584 | 57 | 331 | 399 | 269 | 130 | 59 | 8 | Good | ||||
| [107] | Italy | 68.00 | 6272 | 3968 | 2303 | 3631 | 859 | 1891 | 181 | 9 | Very Good | ||||||||
| [108] | USA | 18472 | 7388 | 11083 | 7388 | 3509 | 2216 | 10 | Very Good | ||||||||||
| [109] | UK | 1200 | 686 | 513 | 645 | 417 | 160 | 206 | 10 | Very Good | |||||||||
| [110] | USA | 73.00 | 206 | 101 | 105 | 152 | 206 | 7131 | 10 | Very Good | |||||||||
| [5] | Spain | 69.10 | 1139 | 695 | 444 | 617 | 310 | 312 | 89 | 9 | Very Good | ||||||||
| [111] | Belgium | 86.00 | 154 | 51 | 103 | 39 | 28 | 181 | 6 | Satisfactory | |||||||||
| [112] | USA | 52.70 | 442 | 256 | 186 | 159 | 84 | 47 | 9 | Very Good | |||||||||
| [113] | UK | 68.00 | 605 | 272 | 333 | 200 | 30 | 90 | 206 | 10 | Very Good | ||||||||
| [114] | UK | 69.30 | 1474 | 787 | 686 | 728 | 228 | 138 | 7131 | 8 | Good | ||||||||
*Abbreviations: No = Number.
Demographic characteristics
Based on the data analysis, the total number of hospitalized patients covered by this analysis was 121,437, which includes 27,062 patients with hypertension, 14,300 patients with diabetes, 9,914 patients with cardiovascular diseases, 9,603 patients with chronic kidney disease, 266 patients with coronary heart disease, and 176 patients with both cardiovascular and cerebrovascular diseases. According to the results, 54.92 percent of the subjects were male (95% CI: 52.92–56.92; I2 = 96.53%), while 45.12 percent were female (95% CI: 43.12–47.12; I2 = 96.55%) (Table 2). The mean age of the subjects in all the included studies was 58.42 years. Most of the studies were conducted in China, while 11 were conducted in the United States, 6 in Italy, 4 in the UK, 2 in Korea, 1 in Spain, 1 in Belgium, 1 in Greece, 1 in Bolivia, and 1 in Singapore. We should also note that six selected studies have not reported the number of patients with both cardiovascular and cerebrovascular disease separately. Based on the papers that reported the number of individuals with a history of exposure, the prevalence of the total exposure history was calculated as 35.56% (95% CI: 21.97–50.38; I2 = 99.43%) (Table 2).

| Number of studies | Prevalence (%) | 95% CI | I2(%) | |
|---|---|---|---|---|
| Sex | ||||
| male | 101 | 54.92 | (52.92–56.92) | 96.53 |
| female | 101 | 45.12 | (43.12–47.12) | 96.55 |
| Exposure history | 21 | 35.56 | (21.97–50.38) | 99.43 |
| Signs and symptoms | ||||
| Fever | 73 | 79.26 | (74.98–83.26) | 97.35 |
| Cough | 71 | 60.70 | (56.91–64.43) | 94.98 |
| Fatigue or Myalgia | 60 | 33.21 | (28.86–37.70) | 96.12 |
| Dyspnea | 61 | 31.30 | (26.14–36.69) | 97.67 |
| Diarrhea | 56 | 10.65 | (8.26–13.27) | 94.20 |
| Comorbidity | 54 | 45.98 | (34.47–57.71) | 99.69 |
| Hypertension | 96 | 28.30 | (23.66–33.18) | 99.58 |
| Cardiovascular and cerebrovascular diseases | 6 | 18.25 | (7.47–32.11) | 94.10 |
| Diabetes | 98 | 14.29 | (11.88–16.87) | 99.10 |
| Chronic kidney disease | 58 | 5.19 | (3.95–6.58) | 96.42 |
| Heart diseases | ||||
| Cardiovascular disease | 68 | 12.30 | (9.59–15.27) | 99.33 |
| Coronary heart disease | 17 | 7.37 | (4.86–10.28) | 86.50 |
| Mortality | 58 | 8.91 | (6.34–11.84) | 98.45 |
Clinical manifestations
The results of this analysis indicate that the prevalence of the most common symptoms of COVID-19 were 79.26% for fever (95% CI: 74.98–83.26; I2 = 97.35%), 60.70% for coughing (95% CI: 56.91–64.43; I2 = 94.98%), 33.21% for fatigue or myalgia (95% CI: 28.86–37.70; I2 = 96.12%), 31.30% for dyspnea (95% CI: 26.14–36.69; I2 = 97.67%), and 10.65% for diarrhea (95% CI: 8.26–13.27; I2 = 94.20%) (Table 2).
Comorbidities
In this systematic review, we focused on the prevalence of people with comorbidities, which was 45.98% (95% CI: 34.47–57.71; I2 = 99.69%) (Table 2). The prevalence of the most common comorbidities were 28.30% for hypertension (95% CI: 23.66–33.18; I2 = 99.58%) (Fig 2, Table 2), 14.29% for diabetes (95% CI: 11.88–16.87; I2 = 99.10%) (Fig 3, Table 2), 12.30% for cardiovascular diseases (95% CI: 9.59–15.27; I2 = 99.33%) (Fig 4, Table 2), and 5.19% for chronic kidney disease (95% CI: 3.95–6.58; I2 = 96.42%) (Table 2). We also assessed the prevalence of some other comorbidities found in our included articles, such as cardiovascular and cerebrovascular diseases with 18.25% (95% CI: 7.47–32.11; I2 = 94.10%), and coronary heart disease with 7.37% (95% CI: 4.86–10.28; I2 = 86.50%) (Table 2).

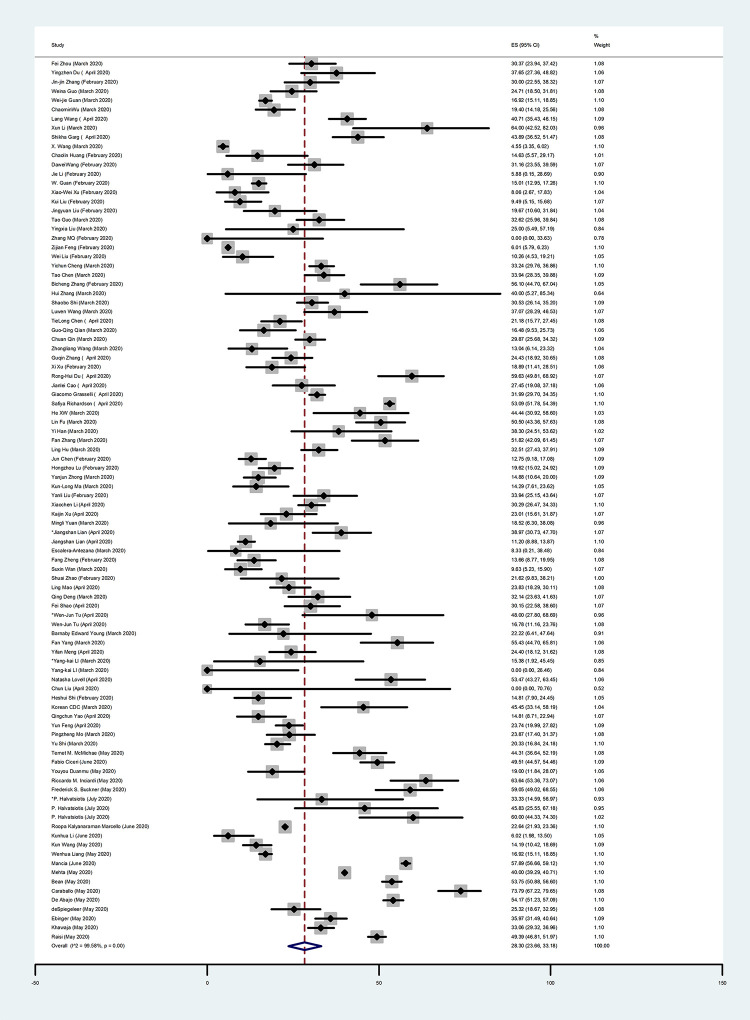
Forest Plot of the prevalence of hypertension in COVID-19 patients.
Each square indicates the effect estimate of individual articles with their 95% CI Size of squares is proportional to the weight of each paper in the meta-analysis. In this plot, papers are indicated in the order of first author’s names and publication date (based on a random effects model).

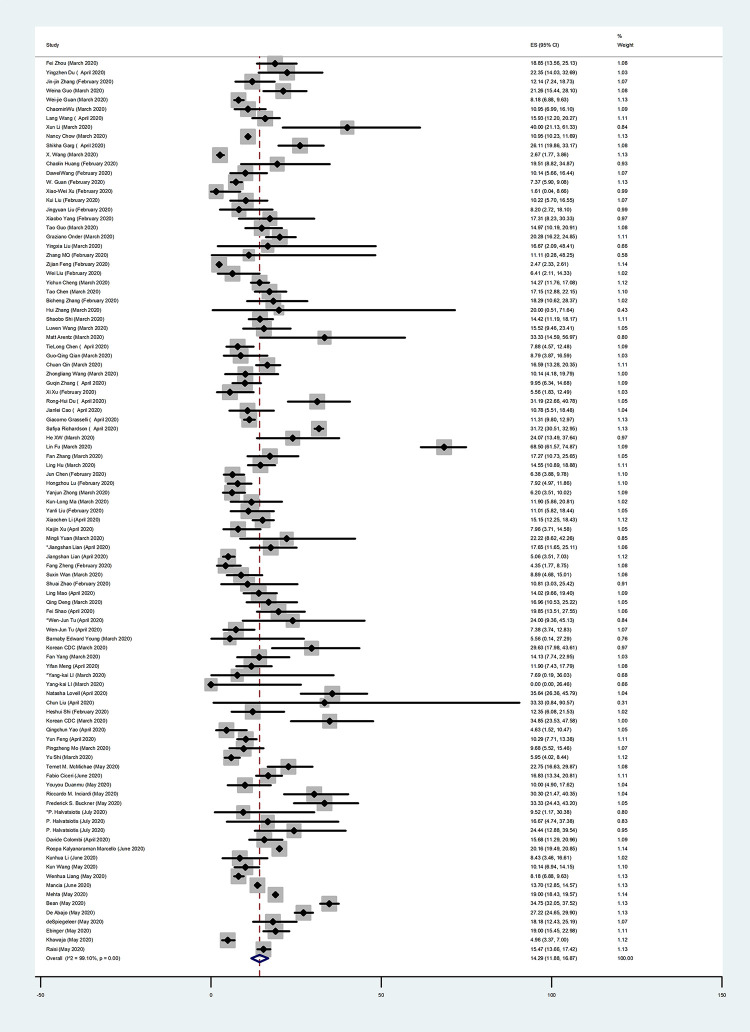
Forest Plot of the prevalence of diabetes in COVID-19 patients.
Each square indicates the effect estimate of individual articles with their 95% CI Size of squares is proportional to the weight of each paper in the meta-analysis. In this plot, papers are indicated in the order of first author’s names and publication date (based on a random effects model).

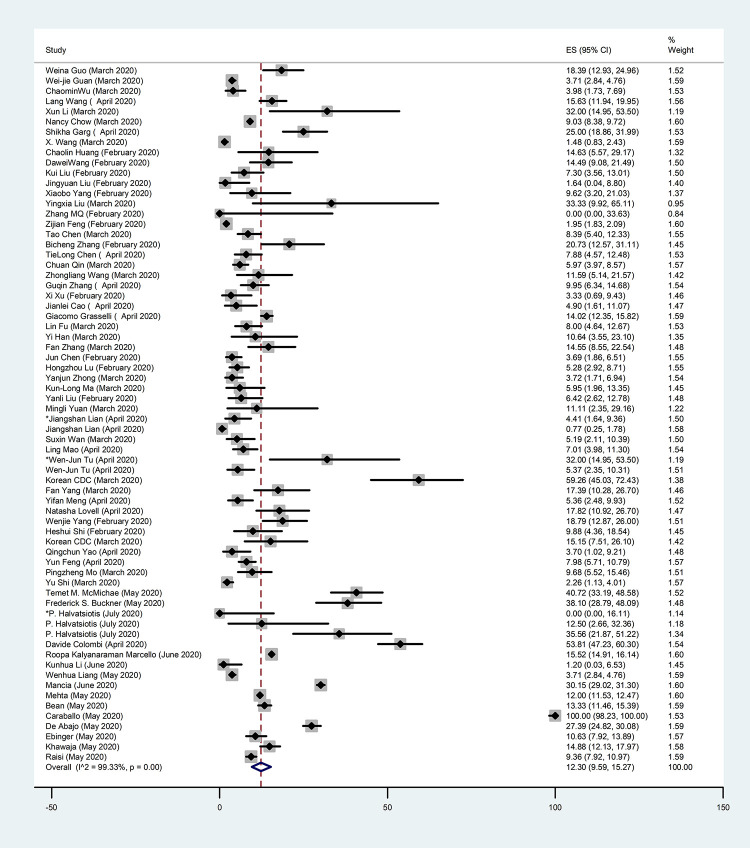
Forest Plot of the prevalence of cardiovascular diseases in COVID-19 patients.
Each square indicates the effect estimate of individual articles with their 95% CI Size of squares is proportional to the weight of each paper in the meta-analysis. In this plot, papers are indicated in the order of first author’s names and publication date (based on a random effects model).
Outcomes
We calculated the percentage of the mortality rate based on all the selected studies reporting mortality cases, and it was 15.18% (95% CI: 10.88–20.02; I2 = 99.19%). After performing the sensitivity analysis and eliminating five studies from our selected studies because they were conducted on deceased individuals, i.e., the outlier studies, the overall mortality rate was calculated based on the remaining 58 studies as 8.91% (95% CI: 6.34–11.84; I2 = 98.45%) (Table 2).
Publication bias
Fig 5 Shows the Begg’s funnel plot of the comorbidity studies performed on patients with COVID-19 infection. The interpretation of our Begg’s funnel plot (p = 0.780), as well as Egger’s test (p = 0.069), shows no sign of publication bias in the included studies. Therefore, it is understandable that reports have been published with both positive and negative outcomes (Fig 5). Based on the results of the meta-regression analysis, the correlation between the prevalence and the sample size was evaluated. Based on this assessment and the figure, there was no significant relation between the prevalence and the sample size (P = 0.428). It should be noted that in this figure, the circles indicate the weight of the papers (Fig 6).

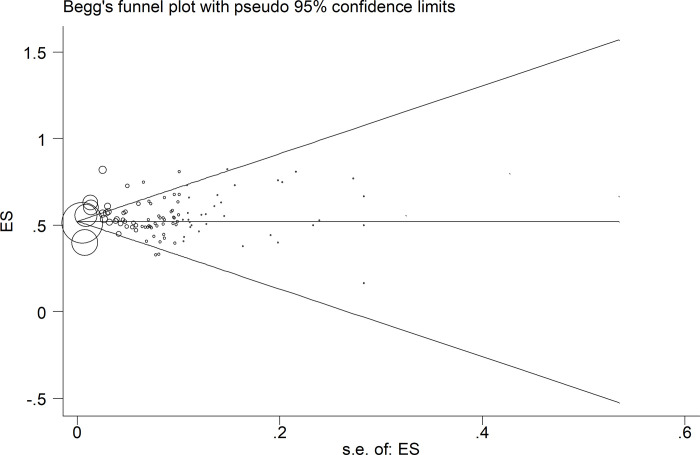
Begg’s funnel plot for publication bias.

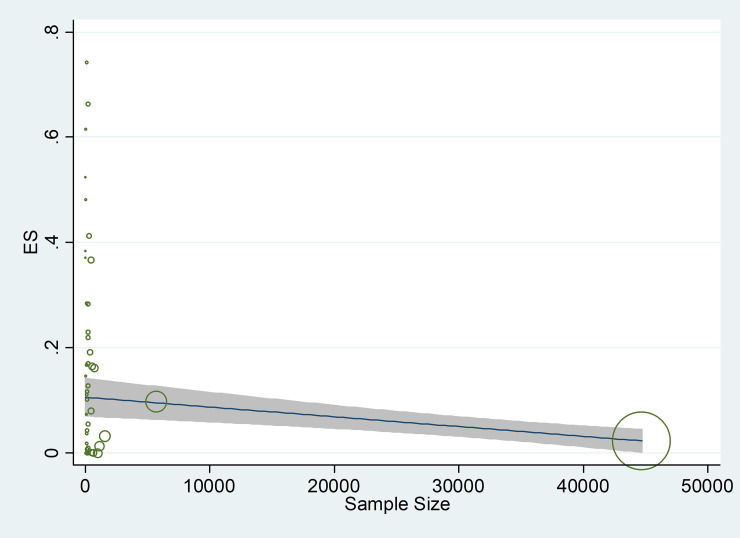
The association between prevalence of risk factors for COVID-19 and sample size, using Meta regression.
In December 2019, a new coronavirus disease, i.e., coronavirus disease 2019 (COVID-19), spread globally [115]. The city of Wuhan in China is considered to be one of the most infected areas in the world [116]. Because of this epidemic contagious disease, aggressive quarantine has been enforced by the government, which has played an important role in monitoring the prevalence of this virus. COVID-19 is not only highly contagious and insidious, but it also has the ability to give rise to cluster outbreaks [117, 118]. The SARS-CoV-2 virus can attack certain cells in the body, particularly alveolar epithelial cells, through a specific enzyme called the angiotensin-converting enzyme 2 (ACE2). ACE2 is considered to be the isoenzyme of ACE, which is mainly distributed in the testes, the kidneys, the colon, the cardiovascular system, the lungs, and other organs [119].
As of the time of writing this review, the pathogenesis and origin of COVID-19 have remained unknown, and no useful medical treatment has been offered for COVID-19 infection. Recommendations insist on intensive supportive care to reduce the risk of infection with this SARS-CoV-2 virus [10, 29]. Unfortunately, in severely-ill COVID-19 patients, the disorder develops rapidly, and the acute respiratory distress syndrome (ARDS), as one of the worst complications of COVID-19 outcomes, can occur earlier and even lead to death. In a study by Tian et al. [120], it was stated that the percentage of mild and seriously-ill patients was 73% and 18%, respectively. Furthermore, Wang et al. found that the risk of exacerbation in patients with cerebrovascular disease, hypertension, cardiovascular disease, or diabetes was higher than others [1].
This meta-analysis is based on data from 102 studies with laboratory-confirmed SARS-CoV-2 cases. The selected studies were from all over the world, and not a specific region. Based on previous studies on SARS-CoV and MERS-CoV, it is understood that these viruses affect males more than females [121, 122]. Moreover, based on our results, men with 54.92% (95% CI: 52.92–56.92; I2 = 96.53%) are more affected by SARS-CoV-2 than women with 45.12% (95% CI: 43.12–47.12; I2 = 96.55%). Furthermore, this may be due to women’s more adaptive innate immune system and robust responses [48]. Another reason for our findings may be that men have a tendency to have more harmful lifestyle habits, such as smoking, as well as underlying diseases, than women [11]. Moreover, as mentioned in Huang’s report [1], this may be associated with the risk factors that are related to men’s occupations, such as the exposure in Huanan wet market. Furthermore, based on our results, older people (mean age = 58.42) are more prone to COVID-19, which could be related to an increase in the frequency of common comorbidities [32]. As our body’s immunity weakens with age, elderly patients are more likely to have serious ailments or even die [11]. Hospitalization and further ICU admission is prevalent among sever cases of COVID-19, especially the ones with underlying health conditions and elderly patients [123]. Based on a CDC report, 8 death cases out of every 10 death cases occurring in the USA are old individuals (i.e., 65 years old and above) [124]. Additionally, it has been reported that patients with comorbid conditions, such as diabetes, hypertension, cardiovascular disease, obesity, and chronic lung diseases, are more likely to have a worse prognosis and develop severe pneumonia and further ARDS [125].
Our study provides satisfactory evidence for the risk factors in severely-ill COVID-19 patients, such as characteristics of the patients (gender, age), comorbidity (hypertension, chronic kidney disease, diabetes, cardiovascular and cerebrovascular diseases, and coronary heart disease), and signs and symptoms (fever, diarrhea, fatigue or myalgia, and dyspnea) [25]. Furthermore, we have discovered that underlying diseases such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease can be considered as risk factors for the progression of this disease, which is confirmed by the analytical results of our study. Moreover, the most common clinical symptoms of COVID-19 in infected patients, including fever, diarrhea, fatigue or myalgia, and dyspnea, have been assessed in this paper. Dyspnea or shortness of breath indicates lack of oxygen and poor lung function. Therefore, if the patient is an elderly male with underlying diseases, he is more likely to have severe disorders or even face death [11].
Neurological complications can also occur as a result of COVID-19; however, they are very rare (especially in contrast to respiratory complications). According to recent reports, neurological manifestations of COVID-19 include headache, vomiting, nausea, dizziness, hyposmia, hypogeusia, and impaired consciousness [12, 78]. Although the exact neuroinvasive route of SARS-CoV-2 has not yet been established, two hypothetical routes have been suggested, i.e., (1) neural dissemination through the olfactory nerve and the cribriform plate, and (2) hematogenous dissemination through cerebral circulation [126, 127]. According to these possible routes, neural invasion of SARS-CoV-2 seems possible. Additionally, it has been proved that there is a close relationship between neurological disorders and COVID-19; however, a big question that arises in this regard is whether this relationship is causal or not (i.e., does one of them affects the mortality rate or the incident of the other one or not?). The answer to this question has not yet been given; however, there is some evidence showing that SARS-CoV-2 infection can affect the clinical spectrum of neurological disorders [128].
According to the selected papers assessed in the current study, fever with 79.26% (95% CI: 74.98–83.26; I2 = 97.35%) is the most common symptom, while hypertension with 28.30% (95% CI: 23.66–33.18; I2 = 99.58%) can be considered as the most prevalent comorbidity. When comparing our results with those of other recent meta-analysis studies, the study conducted by Rodriguez-Morales et al. [129] confirms our findings. These authors found that fever with 88.7% (95% CI 84.5–92.9) was the most prevalent symptom, and hypertension with 18.6% (95% CI 8.1–29.0) was the most common comorbidity. However, the number of selected studies in our meta-analysis was larger than the size of their dataset; hence, our findings are more reliable.
Our findings are also in line with the results of the study by Jing Yang et al. [14], in which fever with 91.3% (95% CI: 86–97) was the most prevalent symptom, and hypertension with 21.1% (95% CI: 13.0–27.2) was the most common comorbidity. In addition, in a study by Emami et al. [130], hypertension was reported as the most prevalent comorbidity with 16.37% (95%CI: 10.15–23.65). Moreover, the prevalence of diabetes mellitus and hypertension in China were 10.9% [131] and 23.2% [132] in adults, respectively.
Based on the abovementioned studies and our results, individuals with cardiovascular diseases, hypertension, chronic kidney disease, and diabetes should receive serious attention for treatments and vaccinations useful for SARS-CoV-2 in the future. Due to limited evidence, more comprehensive studies are needed to demonstrate this correlation [14].
Unfortunately, no anti-virus vaccines or medicines are yet known for the treatment of COVID-19-related diseases. At the present time, clinical management, including infection prevention, supportive care, and control measures, such as mechanical ventilation and supplementary oxygen, are available. Antibiotics are not useful in curing COVID-19 patients; however, they can be employed in the case of a secondary bacterial infection.
Favilavir
Favilavir is an antiviral drug approved in 2014 in Japan as a treatment for influenza. It is currently in use in some countries as a treatment for COVID-19 [133]. Another anti-virus drug which can have useful effects for COVID-19 is called Remdesivir. It has demonstrated efficacy by resisting two viruses that are similar to SARS-CoV2, i.e., MERS-CoV and SARS-CoV in animals [134, 135].
Remdesivir
Remdesivir was employed to cure the first case of COVID-19 infection in the US, resulting in enhancing the conditions of the patient after only one day of using Remdesivir [136]. Based on the related investigations, Remdesivir improved severe lung pathology, reduced lung viral loads, and ameliorated pulmonary function. In addition, chloroquine was suggested in the recommendations for the treatment and prevention of COVID-19 pneumonia [137]. Nevertheless, the optimal dosage of chloroquine for treating SARS-CoV-2 needs to be evaluated in future trials [138]. Hydroxychloroquine is an analog of chloroquine which is used to reduce drug-drug interactions [139]. There is no approved data about the use of corticosteroids for the treatment of SARS-CoV2 [140, 141]. Overall, there is no specific reason yet to expect that patients with COVID- 19 infection will improve by using corticosteroids; hence, these treatments may have harmful effects [142, 143].
A recent clinical trial by [144] suggests that Remdesivir is a therapeutic option for COVID-19 patients who do not receive invasive ventilation. Based on the clinical and experimental results, clinical trials for evaluating the efficacy of Remdesivir in COVID-19 patients have recently been initiated in the USA, China [145, 146], Hong Kong, the Republic of Korea, Singapore [147], Taiwan [148, 149], and France [150, 151].
Lopinavir/Ritonavir
Moreover, based on the investigations, treatment with lopinavir/ritonavir does not decrease the duration of viral RNA or viral RNA loads [11]. In addition, the number of patients treated with lopinavir/ritonavir who developed serious complications, such as secondary infections and acute kidney injury, or who required invasive or noninvasive mechanical ventilation due to respiratory failure, was lower than the number of patients who did not receive lopinavir/ritonavir treatment [11]. These observations need additional studies to find out whether treatment with lopinavir/ritonavir is able to decrease some complications in COVID-19 patients [11, 152].
On February 24, 2020, Moderna Company stated that the company’s experimental mRNA COVID-19 vaccine, which is known as mRNA-1273, was ready to be tested on human subjects. It is a considerably fast progress to produce an initial vaccine just a few weeks after determining the SARS-CoV-2 genetic sequence. However, the clinical trial of the immunogenicity and safety of mRNA-1273 in the treatment of COVID-19 needs to be evaluated more extensively (clinicaltrials.gov Identifier: NCT04283461). Additionally, a new oral SARS-CoV-2 vaccine has been successfully produced at Tianjin University, which employs food-grade safe Saccharomyces cerevisiae as a transporter and targets the S protein. There are 18 biotechnology universities and companies in China studying potential SARS-CoV-2 vaccines [143].
Current diagnostic tests for coronaviruses include real-time RT-PCR (rRT-PCR), reverse transcription loop-mediated isothermal amplification (RT-LAMP), and reverse-transcription polymerase chain reaction (RT-PCR) [153]. RT-LAMP has the same sensitivity as rRT-PCR; however, it is highly particular and is employed to detect MERS-CoV [154, 155]. Based on the current diagnosis represented by the laboratory examinations of the Chinese National Health Commission, oropharyngeal and nasopharyngeal swab tests have become a standard evaluation for the diagnosis of COVID-19 infection. A large portion of the vaccines being produced for coronaviruses target the spike glycoprotein or the S protein [156]. However, vaccine development takes too long, and no vaccines are available at the time of this pandemic [143].
In addition, COVID-19 prevents access to health care for the most vulnerable individuals due to health inequalities [157]. Although structural racism has been shown to affect the distribution of health determinants and risk factors in society, but due to the lack of understanding on the exact influence of these variables on social health, appropriate action is not given by the health system [158, 159]. Focus on addressing both unsupplied social needs (i.e. the immediate social conditions that put the greatest pressure on individuals) and social risk factors (adverse social conditions such as those associated with poor health) can help us solve this problem with a more holistic point of view [158].
Inopportunely, the unfortunate consequences of structural racism, which has been a problem since the days of the transatlantic slave trade, have continued to this day and include a more high poverty rate, an imperfect public school system, police brutality, unsafe neighborhoods and, above all, or, higher rate of chronic health conditions, obesity, and infant and maternal mortality among black American populations [160]. In compatibility with these unfortunate facts, the US national COVID-19 hospitalization rate was 4.6 times higher in Latins and the death rate was 2.1 times higher in black Americans than in whites [161]. Furthermore, it was reported that pregnancy-related complications and further death were three to four times higher in black women than in white women and were also twice as likely to die from heart disease [162–164]. Consequently, a powerful multidisciplinary and coordinated effort must be given by whoever is responsible, including politicians, policy makers, public health professionals, educators and local community leaders, to provide, systematically and actively improve health equity [161].
This data is not incredible or new. Because of these statistics, the chance of death due to pregnancy-related outcomes in black women is three to four times higher than in white women. The probability of death from heart disease in black women is also twice as high as in white women [161, 163, 165, 166]. The Covid-19 epidemic shows the relationship between social risk factors, health and structural racism. The prevalence of diabetes among black Americans has been reported 1.7 times greater than in whites [166]. The prevalence of influenza-related hospitalization in black Americans has been shown to be 1.8 times that of white Americans in the past 10 flu seasons [161]. It has been hypothesized that the increased exposure to COVID-19 among the black American population is due to the higher rate of service occupations and the greater possibility of living in more crowded and dense cities [167–169]. In the current economy, people of color are more likely to lose their jobs due to the potential consequences of the prevalence of COVID-19: 16.8% of black workers and 17.6% of Hispanic workers are at risk of losing their jobs compared to approximately 12.5% of non-Hispanic whites [161]. However, more research is needed for the structural factors leading to these statistics [169].
Early diagnosis and isolation of the patients constitute a key mechanism in preventing the spread of communicable diseases; however, as SARS-Cov-2 has other transmission routes (e.g., fomite transmission), it is even harder to control its rapid global spread [170]. Recently, it has been reported that SARS-CoV-2 is also detectable in saliva, urine, stool, and gastric mucosa [11, 171, 172], which can be related to its high transmission rate. In conclusion, the best protection against infection in the population is improving personal protection and managing hygiene at the community level [170]. According to an experience in Hangzhou City, China, centralized medical observation points (medical observation of close contacts) can also be helpful in controlling the COVID-19 outbreak [173].
In summary, the results of the current review indicate that in COVID-19 patients, diabetes, hypertension, cardiovascular disease, and chronic kidney disease are the most common comorbidities, while fever, diarrhea, fatigue or myalgia, and dyspnea may be considered as the most prevalent symptoms among COVID-19 patients. Since SARS-CoV-2 has a long incubation period and the infected individuals can transmit this contagious virus even without manifesting obvious symptoms, it is highly recommended that sick patients who have underlying disorders, especially in epidemic areas, refrain from coming into contact with other people in the society. Additionally, other strategies, such as avoiding gathering in public areas and going to epidemic places, should be considered as guidelines. During the current COVID-19 outbreak, the reported statistics, related to overall mortality, incubation time, and in particular the risk factors, imply the need for serious decisions for future prevention and therapeutic actions [130].
Conclusions
This systematic review and meta-analysis summarized the current evidence on the prevalence of mortality and potential risk factors in patients with COVID-19. Based on the results of this meta-analysis, COVID-19 is closely associated with underlying diseases. According to our results, the most frequent comorbidities among hospitalized COVID-19 patients were hypertension, diabetes, cardiovascular disease, and chronic kidney disease, respectively. The results also show that old men with underlying diseases are at a higher risk of becoming infected with COVID-19. Therefore, given the high risk of death in patients with COVID-19 infection, special care and significant attention are needed in COVID-19 patients with associated conditions. Moreover, future studies are necessary to identify efficient treatments for severe COVID-19 patients who suffer from diabetes, hypertension, chronic kidney disease, or cardiovascular diseases.
Acknowledgements
The authors of this study are thankful to Shahid Beheshti University of Medical Sciences, Tehran, Iran because of their valuable collaboration and cooperation.
Abbreviations
| WHO | World Health Organization |
| ICU | intensive care unit |
| ACE2 | angiotensin-converting enzyme 2 |
| No | Number |
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
 The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study
The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study
