
Competing Interests: The authors have declared that no competing interests exist.
- Altmetric
Introduction
The numbers of retrieved lymph nodes (RLNs) and positive lymph nodes (PLNs) had a significant impact on the survival of patients with ampulla of vater cancer (AVC), but the optimal numbers of the both were controversial.
Objective
The cohort study aimed to explore the prognostic value and the optimal point of RLNs and PLNs for AVC.
Methods
A total of 2347 AVC patients with M0 disease who underwent surgical resection and lymph node dissection from January 2004 to December 2013 were acquired from a prospective database.
Results
The study found that the optimal cut-off values of RLNs were 18 in the N0 cohort and 16 in N1 or entire cohort due to the highest 5-year overall survival (OS) rate and disease-specific survival (DSS) rate and the separation of survival curves (all P < 0.05). In patients with RLNs ≥ 16, patients with PLN = 0 demonstrated significantly better 5-year OS and DSS rates (70.9% and 77.1%) compared to those with PLNs = 1–2 (41.6% and 44.7%; all P < 0.001), and patients with PLNs = 1–2 demonstrated significantly better 5-year OS and DSS rates (41.6% and 44.7%) compared to those with PLNs ≥ 3 (24.3% and 28.0%; all P < 0.001).
Conclusions
This article recommended that at least 16 lymph nodes will improve the prognosis of AVC patients undergoing surgery. The best cut-off values of PLNs recommended for this study were 0 and 2, which may accurately stratify patients.
Introduction
Ampulla of vater cancer (AVC) was a rare malignancy arising from the papilla of vater [1], and the incidence of AVC in the United States has increased year by year since 1973 [2]. Among periampullary adenocarcinoma, the prognosis of AVC was better than pancreatic head cancer or bile duct cancer [3]. However, lymph node metastasis may exist even in early ampullary carcinoma [4], and the rate of lymph node metastasis has been reported as high as 31.3–58.8% [5–7]. Therefore, lymph node dissection was recommended during surgical resection [8]. Increasing evidence indicated that the numbers of retrieved lymph nodes (RLNs) and positive lymph nodes (PLNs) had a significant impact on the survival of patients with AVC [9–12]. Due to the relative lack of disease, current studies about the effects of RLNs and PLNs on the prognosis of patients with AVC were mostly small sample sizes [9, 12–14], and the optimal numbers of the both were controversial. Thus, the cohort study aimed to explore the prognostic value of RLNs and PLNs for AVC and to determine the optimal point of RLNs and PLNs at the population level through a national database.
Materials and methods
Database and samples
The data from the Surveillance, Epidemiology, and End Results (SEER) database was acquired from the SEER*Stat 8.3.6 Software (https://seer.cancer.gov/data/), and we accessed the SEER database on March 1, 2020. A total of 2875 AVC patients who underwent surgical resection and lymph node dissection (RLNs ≥ 1) from January 2004 to December 2013 were identified by that primary site of tumor was C24.1-Ampulla of Vater, year of diagnosis was from 2004 to 2013, surgery of primary tumor was encoded from 20 to 90 (such as simple/partial surgical removal of primary site, total surgical removal of primary site, radical surgery), number of lymph nodes examined ≥ 1, diagnostic confirmation was positive histology, and type of follow-up expected was active follow-up. A number of 510 patients who < 18 years old or > 80 years old, died within 1 month, and had M1, MX, or NX diseases were excluded. Finally, 2347 AVC patients with M0 disease were included in the study.
The data collected in this study included age at diagnosis, gender, race, marital status at diagnosis, tumor size, tumor grade, lymph node metastasis, number of RLNs and PLNs, adjuvant radiotherapy and chemotherapy.
Statistical analysis
Continuous variables and categorical variables were presented as median (range) and frequency (percentage). Overall survival (OS) and disease-specific survival (DSS) rates were calculated from diagnosis to death due to any reason and from diagnosis to death due to VAC, respectively. The last follow-up time was November 2018. To get the optimal cut-off value of RLNs, the survival analysis performed by Kaplan-Meier method (log-rank test) was compared the 5-year OS and DSS rates of different cut-off values of RLNs in N0, N1 and entire cohorts, respectively, and it was used the 5-year survival rates and P values of different cut-off values of RLNs as line charts. The optimal number of PLNs was gained by X-tile software (Version 3.6.1, Yale University) and verified by the survival analysis. A two-tailed P < 0.05 was considered statistically significant. Statistical analysis was using STATA 16.0 software. Ethics statement was not required for this study, because SEER database was publicly available. In addition, Data-Use Agreements for the 1975–2017 SEER Research Data File and SEER Radiation Therapy and Chemotherapy Information were signed and the database can be accessed.
Results
Baseline characteristics
During the period from January 2004 to December 2013, 2347 AVC patients with M0 disease who underwent surgical resection and lymph node dissection from the SEER database were included in this study (Table 1). The median age at diagnosis was 65 (20–80) years, and male accounted for about 56.8% (1333/2347). The vast majority (78.7%) were white, 7.3% (172/2347) blcak, and 13.9% (327/2347) other. A total of 33255 lymph nodes were examined with a median number of 13 (1–67), and a total of 4105 positive lymph nodes were found with a median number of 1 (0–31). Tumor size for 145 (6.2%) patients was unknown, and the median tumor size for the remaining patients (93.8%) was 21 (1–87) mm. The median follow-up was 39 (2–155) months. As of November 2018, 981 (41.8%) patients were alive and 1366 (58.2%) patients had died. In the entire cohort (n = 2347), the 1-, 3-, and 5-year OS rates were 85.1%, 56.4%, and 45.5%, respectively, and the corresponding DSS rates were 86.8%, 60.0%, and 50.8%, respectively.

| Demographics | Ampulla of vater cancer (n = 2347) |
|---|---|
| Age at diagnosis (years) | 65(20–80) |
| Gender, male/female (%) | 1333(56.8)/1014(43.2) |
| Race, n (%) | |
| white | 1848(78.7) |
| black | 172(7.3) |
| other | 327(13.9) |
| Marital status at diagnosis, n (%) | |
| married | 1509(64.3) |
| single/widowed/divorced | 751(32.0) |
| unkown | 87(3.7) |
| Tumor size (mm) | 21(1–120) |
| Tumor grade, n (%) | |
| well differentiated | 272(11.6) |
| moderately differentiated | 1206(51.4) |
| poorly differentiated | 741(31.6) |
| undifferentiated | 19(0.8) |
| unkown | 109(4.6) |
| Lymph node metastasis, yes/no (%) | 1211(51.6)/1136(48.4) |
| Number of retrieved lymph nodes | 13(1–67) |
| Number of positive lymph nodes | 1(0–31) |
| Adjuvant radiotherapy, yes/no or unkown (%) | 609(25.9)/1738(74.1) |
| Adjuvant chemotherapy, yes/no or unkown (%) | 1073(45.7)/1274(54.3) |
The other comprises American Indian/Alaska Native, Asian/Pacific Islander.
Exploration for the optimal cut-off value of retrieved lymph nodes
For exploring the optimal cut-off value of RLNs, survival analysis was conducted to compared the 5-year OS and DSS rates of different cut-off values of RLNs in N0, N1 and entire cohorts for AVC patients with M0 disease was compared by survival analysis (Table 2), and it was used the 5-year survival rates and P values of different cut-off values of RLNs as line charts (Fig 1). In N0 cohort (n = 1136), the optimal cut-off value of RLNs was 18 due to the highest 5-year OS rate (71.4%) and DSS rate (77.7%) and separation of survival curves between patients with RLNs ≥ 18 and RLNs < 18 (Fig 1A and 1B; all P < 0.001). In N1 cohort (n = 1211), the optimal cut-off value of RLNs was 16 due to the highest 5-year OS rate (34.3%) and the third highest 5-year DSS rate (37.7%) and separation of survival curves between patients with RLNs ≥ 16 and RLNs < 16 (Fig 1C, P = 0.004; Fig 1D, P = 0.005). In the entire cohort (n = 2347), the optimal cut-off value of RLNs was 16 due to the highest 5-year OS rate (49.0%) and DSS rate (53.6%) and separation of survival curves between patients with RLNs ≥ 16 and RLNs < 16 (Fig 1E, P = 0.008; Fig 1F, P = 0.015).

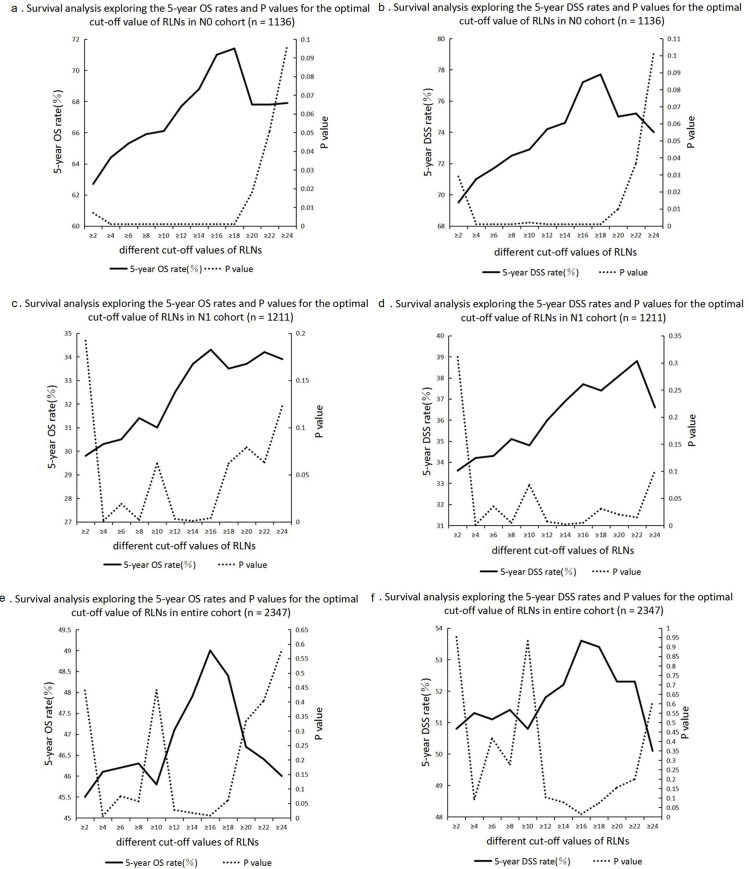
Survival analysis comparing the different numbers of PLNs.
a: Survival analysis exploring the 5-year OS rates and P values for the optimal cut-off value of RLNs in N0 cohort (n = 1136). b: Survival analysis exploring the 5-year DSS rates and P values for the optimal cut-off value of RLNs in N0 cohort (n = 1136). c: Survival analysis exploring the 5-year OS rates and P values for the optimal cut-off value of RLNs in N1 cohort (n = 1211). d: Survival analysis exploring the 5-year DSS rates and P values for the optimal cut-off value of RLNs in N1 cohort (n = 1211). e: Survival analysis exploring the 5-year OS rates and P values for the optimal cut-off value of RLNs in entire cohort (n = 2347). f: Survival analysis exploring the 5-year DSS rates and P values for the optimal cut-off value of RLNs in entire cohort (n = 2347).

| Retrieved lymph nodes | N | Overall Survival (OS) | Disease-specific survival (DSS) | ||
|---|---|---|---|---|---|
| 5-year OS rate (%) | P value | 5-year DSS rate (%) | P value | ||
| In N0 cohort | 1136 | ||||
| < 2 | 44 | 49.8 | 0.007 | 57.8 | 0.029 |
| ≥ 2 | 1092 | 62.7 | 69.5 | ||
| < 4 | 136 | 46.9 | <0.001 | 55.1 | <0.001 |
| ≥ 4 | 1000 | 64.4 | 71.0 | ||
| < 6 | 241 | 51.1 | <0.001 | 59.5 | 0.001 |
| ≥ 6 | 895 | 65.3 | 71.7 | ||
| < 8 | 361 | 54.4 | <0.001 | 61.7 | <0.001 |
| ≥ 8 | 775 | 65.9 | 72.5 | ||
| < 10 | 479 | 57.0 | <0.001 | 63.9 | 0.002 |
| ≥ 10 | 657 | 66.1 | 72.9 | ||
| < 12 | 585 | 57.1 | <0.001 | 64.3 | <0.001 |
| ≥ 12 | 551 | 67.7 | 74.2 | ||
| < 14 | 692 | 58.2 | <0.001 | 65.6 | <0.001 |
| ≥ 14 | 444 | 68.8 | 74.6 | ||
| < 16 | 785 | 58.4 | <0.001 | 65.5 | <0.001 |
| ≥ 16 | 351 | 71.0 | 77.2 | ||
| < 18 | 862 | 59.4 | <0.001 | 66.4 | <0.001 |
| ≥ 18 | 274 | 71.4 | 77.7 | ||
| < 20 | 929 | 61.0 | 0.018 | 67.8 | 0.010 |
| ≥ 20 | 207 | 67.8 | 75.0 | ||
| < 22 | 987 | 61.4 | 0.051 | 68.2 | 0.037 |
| ≥ 22 | 149 | 67.8 | 75.2 | ||
| < 24 | 1030 | 61.6 | 0.097 | 68.6 | 0.102 |
| ≥ 24 | 106 | 67.9 | 74.0 | ||
| In N1 cohort | 1211 | ||||
| < 2 | 7 | 14.3 | 0.192 | 19.0 | 0.311 |
| ≥ 2 | 1204 | 29.8 | 33.6 | ||
| < 4 | 48 | 15.1 | 0.001 | 18.7 | 0.001 |
| ≥ 4 | 1163 | 30.3 | 34.2 | ||
| < 6 | 113 | 21.7 | 0.019 | 27.3 | 0.035 |
| ≥ 6 | 1098 | 30.5 | 34.3 | ||
| < 8 | 198 | 21.3 | 0.002 | 25.5 | 0.005 |
| ≥ 8 | 1013 | 31.4 | 35.1 | ||
| < 10 | 304 | 25.7 | 0.062 | 29.9 | 0.075 |
| ≥ 10 | 907 | 31.0 | 34.8 | ||
| < 12 | 434 | 24.9 | 0.003 | 29.3 | 0.007 |
| ≥ 12 | 777 | 32.5 | 36.0 | ||
| < 14 | 557 | 25.2 | 0.001 | 29.8 | 0.002 |
| ≥ 14 | 654 | 33.7 | 36.9 | ||
| < 16 | 684 | 26.4 | 0.004 | 30.5 | 0.005 |
| ≥ 16 | 527 | 34.3 | 37.7 | ||
| < 18 | 787 | 27.8 | 0.062 | 31.5 | 0.031 |
| ≥ 18 | 424 | 33.5 | 37.4 | ||
| < 20 | 877 | 28.2 | 0.079 | 31.9 | 0.020 |
| ≥ 20 | 334 | 33.7 | 38.1 | ||
| < 22 | 951 | 28.5 | 0.063 | 32.1 | 0.015 |
| ≥ 22 | 260 | 34.2 | 38.8 | ||
| < 24 | 1019 | 28.9 | 0.123 | 33.0 | 0.101 |
| ≥ 24 | 192 | 33.9 | 36.6 | ||
| In entire cohort | 2347 | ||||
| < 2 | 51 | 44.9 | 0.440 | 52.6 | 0.953 |
| ≥ 2 | 2296 | 45.5 | 50.8 | ||
| < 4 | 184 | 38.6 | 0.006 | 45.6 | 0.093 |
| ≥ 4 | 2163 | 46.1 | 51.3 | ||
| < 6 | 354 | 41.7 | 0.075 | 49.2 | 0.416 |
| ≥ 6 | 1993 | 46.2 | 51.1 | ||
| < 8 | 559 | 42.8 | 0.057 | 49.1 | 0.278 |
| ≥ 8 | 1788 | 46.3 | 51.4 | ||
| < 10 | 783 | 44.9 | 0.441 | 50.9 | 0.932 |
| ≥ 10 | 1564 | 45.8 | 50.8 | ||
| < 12 | 1019 | 43.4 | 0.027 | 49.6 | 0.104 |
| ≥ 12 | 1328 | 47.1 | 51.8 | ||
| < 14 | 1249 | 43.4 | 0.017 | 49.7 | 0.077 |
| ≥ 14 | 1098 | 47.9 | 52.2 | ||
| < 16 | 1469 | 43.5 | 0.008 | 49.2 | 0.015 |
| ≥ 16 | 878 | 49.0 | 53.6 | ||
| < 18 | 1649 | 44.3 | 0.061 | 49.8 | 0.074 |
| ≥ 18 | 698 | 48.4 | 53.4 | ||
| < 20 | 1806 | 45.1 | 0.334 | 50.4 | 0.156 |
| ≥ 20 | 541 | 46.7 | 52.3 | ||
| < 22 | 1938 | 45.2 | 0.405 | 50.5 | 0.200 |
| ≥ 22 | 409 | 46.4 | 52.3 | ||
| < 24 | 2049 | 45.4 | 0.579 | 50.9 | 0.611 |
| ≥ 24 | 298 | 46.0 | 50.1 | ||
Exploration for the optimal cut-off value of positive lymph nodes
The media numbers of PLNs were 1 (0–31) in the entire cohort (n = 2347) and 1 (0–31) in patients with RLNs ≥ 16 (n = 878). Whether in the entire cohort or in patients with RLNs ≥ 16, the optimal cut-off values of PLNs were 0 and 2 obtained by X-tile software. In the entire cohort (n = 2347), patients with PLN = 0 demonstrated significantly better 5-year OS and DSS rates (62.1% and 68.9%) compared to those with PLNs = 1–2 (36.4% and 40.4%; Fig 2A and 2B; all P < 0.001), and patients with PLNs = 1–2 demonstrated significantly better 5-year OS and DSS rates (36.4% and 40.4%) compared to those with PLNs ≥ 3 (21.7% and 25.3%; Fig 2A and 2B; all P < 0.001). In patients with RLNs ≥ 16 (n = 878), patients with PLN = 0 demonstrated significantly better 5-year OS and DSS rates (70.9% and 77.1%) compared to those with PLNs = 1–2 (41.6% and 44.7%; Fig 2C and 2D; all P < 0.001), and patients with PLNs = 1–2 demonstrated significantly better 5-year OS and DSS rates (41.6% and 44.7%) compared to those with PLNs ≥ 3 (24.3% and 28.0%; Fig 2C and 2D; all P < 0.001).

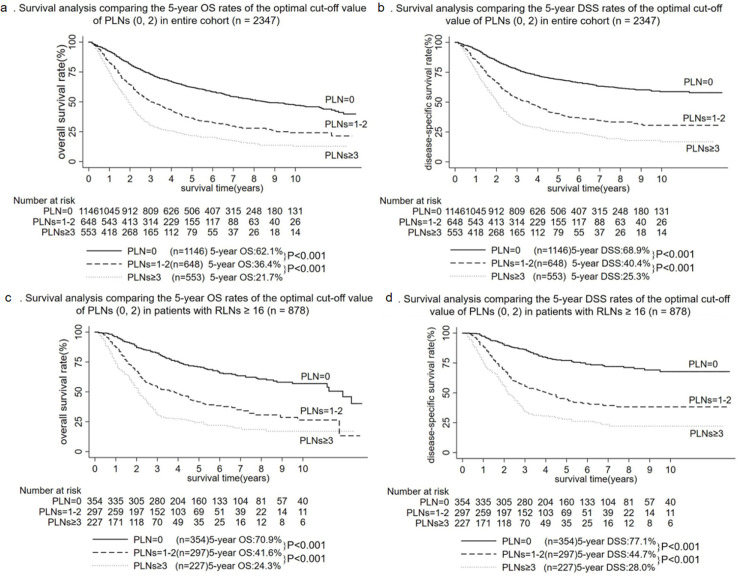
Survival analysis comparing the different numbers of PLNs.
a: Survival analysis comparing the 5-year OS rates of the optimal cut-off value of PLNs (0, 2) in entire cohort (n = 2347). b: Survival analysis comparing the 5-year DSS rates of the optimal cut-off value of PLNs (0, 2) in entire cohort (n = 2347). c: Survival analysis comparing the 5-year OS rates of the optimal cut-off value of PLNs (0, 2) in patients with RLNs ≥ 16 (n = 878). d: Survival analysis comparing the 5-year DSS rates of the optimal cut-off value of PLNs (0, 2) in patients with RLNs ≥ 16 (n = 878).
Discussion
The numbers of RLNs and PLNs were important predictors of survival in patients with AVC [9–12], but it was controversial. Therefore, the end of this study was to explore the prognostic value of RLNs and PLNs for AVC and to determine the optimal point of the both through a national database.
The optimal cut-off value of RLNs supported by this study was 16. Adequate lymph node dissection may improve the prognosis of patients undergoing radical surgery for malignant tumors. Thus, routine lymph node dissection was recommended in AVC patients who underwent surgery [8], whereas there was some controversy over the specific number of RLNs [12, 13]. By comparing the 5-year OS and DSS rates of different cut-off values of RLNs in 2347 M0 patients with AVC who underwent surgical resection and lymph node dissection, the study found that the best cut-off values of RLNs were 18 in N0 cohort and 16 in N1 or entire cohort (Table 2). Overall, this study supported the optimal cut-off value of RLNs of 16 due to the highest 5-year OS rate (49.0%) and DSS rate (53.6%) and separation of survival curves between patients with RLNs ≥ 16 and RLNs < 16 in entire cohort (Fig 1E, P = 0.008; Fig 1F, P = 0.015), which was consistent with the results of a study by Falconi et al. [12]. Falconi et al. [12] found that AVC patients with RLNs ≥ 16 had a good prognosis. However, a single-center study from Europe supported an optimal cut-off value of RLNs of 12, whereas the sample size of the study was only 127 and the method of assigning cut-off values was not objective [13]. Moreover, it seemed feasible to examine at least 16 lymph nodes in patients with AVC because some studies reported that the median RLNs were around 16 [12, 14–16]. In addition, the prognosis of patients with malignant tumor may be better because more lymph nodes were removed. Therefore, this study recommended removing at least 16 lymph nodes.
The best cut-off values of PLNs recommended for this study were 0 and 2. Although there were many predictors affecting the prognosis of AVC, such as age [17], tumor size [10], and differentiation [1], lymph node status was recognized as a key factor affecting the prognosis of the patients [6, 10, 18–20]. The prognosis of AVC patients was poor as the number of positive lymph nodes increased [9, 10]. Bourgouin et al. [9] found that 5-year disease-free survival rates were statistically different among 55 AVC patients with PLN = 0, PLNs = 1–3, and PLNs ≥ 4. But the study of 2347 M0 patients with AVC found that the optimal cut-off values of PLNs were 0 and 2 whether in the entire cohort or in patients with RLNs ≥ 16. Moreover, a study including 1057 AVC patients who underwent surgical resection and had at least 12 lymph nodes examined found that the lymph node classification of AVC should be N0 (PLN = 0), N1 (PLNs = 1–2) and N2 (PLNs ≥ 3) [11], which were consistent with the results of our research. In summary, the best cut-off values of PLNs recommended for this study were 0 and 2.
This study had several limitations. Firstly, although the median number of RLNs in this series was 13, the number of RLNs in some patients was lower, which may hinder the full assessment of lymph node status and affect overall results. Secondly, since the SEER database lacked certain factors that affect the prognosis, such as surgical margins and specific sites of lymph node involvement, a multivariate analysis was not performed in this study, which may affect the results of this study. Thirdly, while we performed a comprehensive verification of the optimal cut-off value of PLNs calculated by software, any software had its shortcomings. New tools or methods for more comprehensive evaluation of optimal cut-off value may be produced in the future, which may affect the results of this study. Nevertheless, research based on a national database could provide greater generality to the results of this study.
Conclusions
This study recommended that at least 16 lymph nodes will improve the prognosis of patients with AVC undergoing surgery. The best cut-off values of PLNs recommended for this study were 0 and 2, which may accurately stratify patients.
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
 Prognostic importance of numbers of retrieved lymph nodes and positive lymph nodes for ampulla of vater cancer (AVC) in 2347 patients from the Surveillance, Epidemiology, and End Results (SEER) database
Prognostic importance of numbers of retrieved lymph nodes and positive lymph nodes for ampulla of vater cancer (AVC) in 2347 patients from the Surveillance, Epidemiology, and End Results (SEER) database
