
- Altmetric
To the editor
We read with interest the study by Thaunat et al. that identified significant excess mortality attributed to coronavirus disease 2019 (COVID-19) among dialysis patients.1 Indeed, the COVID-19 pandemic has provided the impetus for the introduction of strategies to optimize protection of hemodialysis patients from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).2 Outside the pandemic setting, however, patients with chronic kidney disease have significantly higher risk of nosocomial acquisition of other common respiratory-viral infections (RVIs), with increased mortality and length-of-stay.3 Implementation of protective strategies against COVID-19 on renal units may reduce health care–associated-RVI (HA-RVI) as a positive consequence.
From January to December 2020, a COVID-19 containment strategy was implemented at the largest tertiary hospital in Singapore, with a 20-station inpatient dialysis center, a large renal inpatient service, and a renal transplant program. Universal masking and visitor screening were implemented4; symptomatic patients were segregated in a dedicated dialysis room, with staff using personal protective equipment. All symptomatic inpatients were tested for SARS-CoV-2 and common RVIs via multiplex polymerase chain reaction.
The incidence of HA-RVI during the pandemic dramatically decreased to 0.5 cases per 1000 admissions (1 case, 2186 admissions), compared with 21.7 cases per 1000 admissions (70 cases, 3223 admissions) over the previous 2 years (incidence rate ratio, 0.02; 95% confidence interval, 0.001–0.13; P < 0.001). Notably, zero episodes of HA-RVI were recorded from February to December 2020 (Figure 1 ). There was no significant difference in the proportion of inpatients tested for common RVIs (26.5%, 581 of 2186 admissions tested during the pandemic; vs. 28.8%, 929 of 3223 admissions tested prepandemic; odds ratio, 0.89; 95% confidence interval, 0.77–1.08; P = 0.07). Despite managing ≥1600 COVID-19 cases, there was no nosocomial acquisition. Infection prevention measures introduced for COVID-19 mitigate HA-RVI among renal inpatients and should be continued postpandemic.

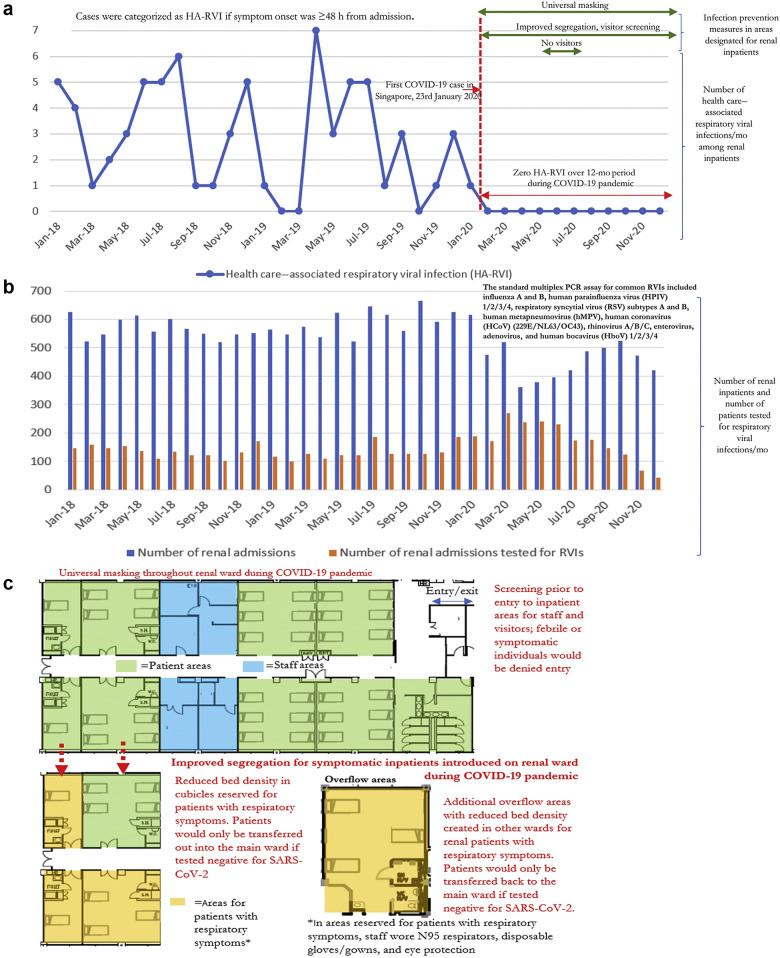
Rates of health care–associated respiratory viral infections (HA-RVIs) among renal inpatients at a Singaporean tertiary hospital, before and during coronavirus disease 2019 (COVID-19) pandemic. (a) Trends in HA-RVIs among renal inpatients (January 2018–December 2020). (b) Number of renal inpatients and number of patients tested for respiratory viral infections (RVIs) at a Singaporean tertiary hospital (January 2018–December 2020). (c) Layout of renal inpatient unit and enhanced infection prevention measures introduced during the COVID-19 pandemic. PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
References
1
2
3
Acknowledgments
As this study utilized aggregated anonymized data collected as part of routine surveillance, waiver of informed consent was obtained from our hospital’s institutional review board.
Author Contributions
WLE conceived and designed the study. WLE and EPC analyzed the data. WLE, CST, and IV drafted the manuscript. CST and IV supervised.
 Zero health care–associated respiratory viral infections: impact of enhanced infection prevention on a renal unit during the coronavirus disease 2019 pandemic
Zero health care–associated respiratory viral infections: impact of enhanced infection prevention on a renal unit during the coronavirus disease 2019 pandemic