- Altmetric
The coronavirus disease 2019 (COVID-19) pandemic is causing extreme stress to many health systems and an ever-mounting death toll. Out of the darkness of the last 14 months comes a beacon of hope in the form of multiple severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines. To best utilize this precious resource, we must efficiently deploy vaccination to high-risk groups.
Providing equitable access to vaccines requires multiple considerations, including quantification of the risk of serious disease according to age and comorbidities, the safety and efficacy of the vaccines, and operational considerations relating to vaccine availability and administration. This editorial aims to highlight both the catastrophic risks of infection with SARS-CoV-2 and of subsequent death from COVID-19 in dialysis patients and the current failure to recognize these risks when considering priorities for COVID-19 vaccination. This is a “Call to Action” for policy makers worldwide to ensure prioritized designation of these patients in their countries.
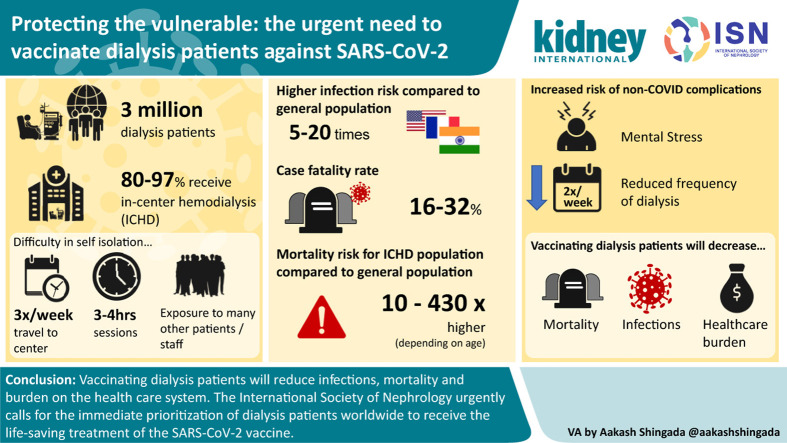
People receiving dialysis treatment for end-stage kidney disease have specific circumstances that lead to an increased risk of SARS-CoV-2 infection. Most patients receive in-center hemodialysis (ICHD), which necessitates traveling to the dialysis center 3 times a week, attending for at least 3 to 4 hours, generally surrounded by numerous other patients as well as staff. Therefore, these patients cannot self-isolate. As an example, patients receiving ICHD in Flanders, France, and in New York, New York, USA, were 5 to 16 times more likely to be diagnosed with COVID-19 disease compared with the general population.1 , S1–S3 Reports from France, England, Belgium, Italy, and the United States during a 4- to 15-week interval in the first COVID-19 surge showed 5% to 20% of ICHD patients were infected with SARS-CoV-2 in this short period.1 , 2 , S1 , S3–S6 Asymptomatic infection and limitations in testing suggest the infected population was even larger, with serologic studies from London, UK, and New York ICHD units revealing a 28% to 36% seroprevalence rate, increasing to 70% in a dialysis unit serving a rehabilitation center.S7 , S8 Similar data have been reported from low- and middle-income countries. Longer-term data from a large network in India revealed 9% of hemodialysis patients tested positive between March and December 2020, a rate 20 times higher than the general population.
Moreover, as well as being especially susceptible to infection because they cannot self-isolate, people receiving ICHD who develop COVID-19 are at least 30% to 130% more likely to die (after adjusting for age) than hospitalized patients with COVID-19 but no chronic kidney disease,1 , S3 , S9–S11 with case fatality rates varying from 16% to 32%.1 , 3 , 4 , S1 , S2 , S4 , S11–S13 The higher risk of death once infected for dialysis patients may be due to impaired immune function and an increased prevalence of other well-established risk factors for death from COVID-19, including hypertension, obesity, diabetes, and heart disease.3 , 4 , S1 , S2 , S4 , S11 , S12 , S14 In addition, the prevalence of kidney failure is higher in Black, Asian, and minority ethnic groups and individuals with low socioeconomic status, groups that have a higher disease burden from COVID-19, where reported. The increased incidence of SARS-CoV-2 infection and increased mortality when infected have resulted in widespread death, with 1 in 33 ICHD patients in the United Kingdom dying from COVID-19 in the first wave.5 Population-based analysis shows age-matched relative risk of death from COVID-19 for an ICHD patient compared with the general population ranges from 432 for a 20- to 39-year-old patient to around 10 for a patient aged >80 years.5
To date, therefore, there is clear evidence that nonelderly patients on dialysis have experienced exceptionally high mortality rates, in most cases equaling or exceeding rates observed in elderly patients in their regions (i.e., those aged >80 years), who (properly) have generally been given priority for vaccination. There is a common misconception that most dialysis patients are very elderly and thus will automatically qualify for immediate vaccination. In fact, dialysis patients are on average younger (mean age, 65–70 years) than the classic high-risk group of those aged ≥85 years, with large potential gains in life years saved by the vaccine. In many countries, patients on dialysis have been placed on equal priority with risk groups, such as those with obesity, heart disease, or diabetes or smokers, which represent a large proportion of the population.S15 Immunizing this enormous group will take time. We argue patients on dialysis should be prioritized, as they are at much greater risk of acquiring COVID-19 than these aforementioned groups and, once infected, their risk of death due to COVID-19 is substantially greater.S16
There are also underrecognized indirect effects of the SARS-CoV-2 pandemic in dialysis patients. The constant threat of death from contracting SARS-CoV-2, particularly at a dialysis session, has led to widespread fear and anxiety for people on dialysis.S17 For this reason, people may skip dialysis sessions, increasing the risk of death, even in the absence of COVID-19 disease. In addition, the general health system strain and the complexities of isolating SARS-CoV-2–positive ICHD patients during surges forced some dialysis units to decrease the number of weekly sessions from 3 to 2, further impacting patient care.S18
There is some nihilism within the medical community regarding vaccination of dialysis patients due to scarce data on the safety and effectiveness of SARS-CoV-2 vaccines in this population. Remarkably, no dialysis patient has been reported to have been included in any of the vaccine trials globally. This obvious “renalism” should not be allowed to translate into vaccination efforts. Limited data from New York report all surviving patients with polymerase chain reaction–confirmed COVID-19 disease had SARS-CoV-2 IgG detectable around 2 months post infection, suggesting seroconversion from a vaccine will occur.S19 Vaccinations against hepatitis B, influenza, and pneumococcal disease are routinely recommended in people receiving maintenance hemodialysis.S20 Seroconversion rates of 33% to 80% are reported for the influenza vaccine, with older patients less likely to seroconvert.S20 Some people, especially elderly patients, require larger doses to effectively seroconvert, and this should be monitored for the SARS-CoV-2 vaccine, as adapted immunization protocols may be required. There is an urgent need to initiate detailed studies of the efficacy of SARS-CoV-2 vaccination among patients with kidney failure (and those who have a functioning kidney transplant).
Dialysis patients are high health care utilizers, allowing for efficient communication regarding the vaccine and any vaccine hesitancy. Frequent in-center attendance eases barriers of vaccine delivery and administration, which can be provided during routine dialysis sessions. The opportunity for mass vaccination at dialysis units provides an unprecedented opportunity for operational efficiency, as all attendees at a dialysis unit could be administered their first dose within 2 days. This would, in turn, protect the families of dialysis patients from exposure to SARS-CoV-2.
Administrators must use evidence-based prioritization for vaccination rather than “one size fits all” approach for patients at the highest risk. As dialysis patients are at the highest risk from COVID-19 (Table 1 ), vaccinating dialysis patients may have the highest relative impact of all health care groups, through reducing infections, mortality, and burden on the health care system. Particular considerations are required for the delivery of vaccination in resource-constrained countries.S21

| Reason | Risk estimates | High-risk groups |
|---|---|---|
| Increased risk of SARS-CoV-2 infection | 5–20 times more likely to be infected than the general population 5%–20% symptomatic and 28%–36% with serologic evidence of infection during the first waveS1,S3–S6 | In-center hemodialysis Diabetes Obesity Lack of private transportationS3,S8 |
| Increased case fatality from COVID-19 | 16%–32% case fatalityS1,S2,S4,S11–S13 50% mortality for those in ICUS10 1.3–2.3 times higher case fatality than hospitalized patients with COVID-19 but no CKD | Hypertension Obesity Older people Heart diseaseS9,S12 |
| High risk of infection and high risk of death once infected translates to high(est) community risk group for death | Relative risk of death compared with age-matched general population5: 20–39 yr: 432 40–59 yr: 94 60–79 yr: 33 >80 yr: ∼10 |
CKD, chronic kidney disease; COVID-19, coronavirus disease 2019; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
People receiving maintenance dialysis report profound psychosocial stress related to the pandemicS17 and anxiously await vaccination. The International Society of Nephrology urgently calls for the immediate prioritization of dialysis patients worldwide to receive the life-saving treatment of the SARS-CoV-2 vaccine. National and regional stakeholders can advocate for priority access to vaccination for dialysis patients and assist efficient implementation of a vaccine program that will protect the most vulnerable: those on dialysis.
Disclosure
All the authors declared no competing interests.
References
1
2
3
4
5
Acknowledgements
The authors gratefully acknowledge the assistance of Drs. Alan Salama, Katie Vinen, and Aakash Shingada in the creation of this article and visual abstract.
Supplementary References.:
 The urgent need to vaccinate dialysis patients against severe acute respiratory syndrome coronavirus 2: a call to action
The urgent need to vaccinate dialysis patients against severe acute respiratory syndrome coronavirus 2: a call to action