
To the editor:
Several reports have described multisystem inflammatory syndrome in children (MIS-C) following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.1 Clinical presentation consists of a hyperinflammatory syndrome and multiorgan involvement, including gastrointestinal symptoms (diarrhea/abdominal pain), hemodynamic instability, myocarditis, cutaneous manifestations, and increased inflammatory markers.2 Delayed inflammatory syndromes have been similarly recognized in adults (MIS-A), with fewer than 30 cases previously reported.3 , 4 We herein describe the first relapsing form of MIS-A post–coronavirus disease 2019 (COVID-19) pneumonia in a kidney transplant recipient.
A 72-year patient was admitted to our unit for COVID-19 pneumonia. In 2006, he received a first kidney transplant for hypertension-related end-stage renal disease. Induction immunosuppressive therapy included basiliximab, and maintenance regimen was cyclosporine, mycophenolic acid, and steroids. Basal creatinine level was 160 μmol/l. He had no other comorbidities but hypertension.
He presented on March 28 with fever, peaking at 39 °C soon after his admission. COVID-19 pneumonia was diagnosed by the presence of a positive SARS-CoV-2 on reverse transcriptase polymerase chain reaction testing performed on nasopharyngeal swab associated to typical computed tomography scan images. Initial treatment included oxygen therapy (3 l/min), azithromycin, and ceftriaxone. The respiratory function deteriorated with increased need for oxygen (6 l/min) and worsening of radiologic infiltration on computed tomography scan. A single infusion of tocilizumab and 20 mg of dexamethasone were then instituted on April 2 followed by high-dose steroid therapy (0.75 mg/kg of prednisone) on April 11 with subsequent tapering over the following 3 weeks. Mycophenolic acid and cyclosporine were withdrawn the day of admission.
Two days after steroids onset, the patient significantly reduced his oxygen need and promptly recovered thereafter. Immunosuppression was reintroduced, and he was discharged from hospital on April 28.
Intermittent fever, rising up to 40 °C, recurred on May 14 in association with de novo atrial fibrillation and bilateral gonalgia, without any other symptoms. Reverse transcriptase polymerase chain reaction to SARS-CoV2 was negative and lung infiltration on chest computed tomography had dramatically improved compared to the initial phase. Anti-SARS-CoV-2 IgG were positive. Blood tests disclosed elevated inflammatory markers (C-reactive protein at 150 mg/l, ferritin up to 3749 μg/l, and interleukin-6 at 629 pg/ml) (Figure 1 ) associated with cytolytic hepatitis (alanine aminotransferase >10× upper limit of normal). Serum C4 and CH50 were decreased (42 mg/l and 19%, respectively), with normal C3 (1170 mg/l). Extensive screening for infections (particularly endocarditis), hematological malignancies, solid cancer, and autoimmunity remained negative. We hypothesized that the inflammatory syndrome could result from the previous SARS-CoV-2 infection (MIS-A) and a course of high-dose i.v. Ig (2 g/kg) was administered. Fever and gonalgia disappeared in a day, while inflammatory markers and hepatic enzymes returned to normal ranges within a few days following i.v. Ig. Interleukin-6 dropped to 23.4 pg/ml.

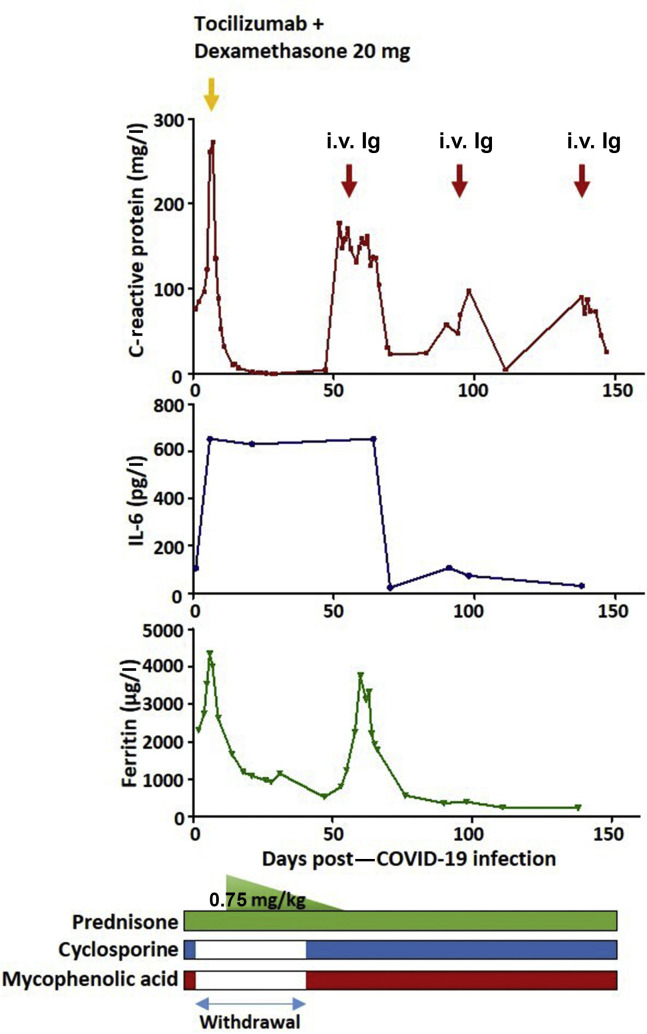
Evolution of serum inflammation markers after coronavirus disease 2019 (COVID-19) pneumonia episode.
One month later, the patient presented with a milder episode that combined fever and inflammatory syndrome (Figure 1), yet without hepatic cytolysis. An etiologic work-up failed to identify any other cause than MIS-A. Then, i.v. Ig was administered for the second time, leading to the prompt resolution of the fever and normalization of inflammatory markers. A third episode occurred 3 weeks later (Figure 1) and similarly responded to i.v. Ig. Reverse transcriptase polymerase chain reaction for SARS-CoV-2 has remained consistently negative at each test following the first discharge. At last follow-up, on November 28, the patient remained free of any fever or other inflammatory signs.
This is the first case of MIS-A associated with COVID-19 in a kidney transplant recipient. Interestingly, 2 relapsing episodes occurred and were resolutive with i.v. Ig. MIS-A is seldom reported and is currently defined as an illness requiring hospitalization in a person older than 21 years with a positive test for current or previous SARS-CoV-2 infection within the preceding 12 weeks, severe extrapulmonary organ dysfunction (cardiac, gastrointestinal, dermatologic, or neurologic symptoms), associated with laboratory markers consistent with hyperinflammation in the absence of severe respiratory symptoms.4 Pathogenesis of MIS, regardless of patient age, is still unknown. A role of autoimmunity induced by SARS-CoV-2 has been proposed in children.5 In our case, the activation of classical complement pathway suggests an immune-complex–mediated mechanism.
In conclusion, the diagnosis of MIS-A should be considered in the settings of unexplained inflammatory syndrome in kidney transplant recipients following COVID-19, after the elimination of differential diagnosis, especially infections. Administration of i.v. Ig may be effective at controlling the clinical and biological signs of inflammation.
1
2
3
4