
These authors contributed equally to this work as first authors
Decision making in immuno‐oncology is pivotal to adapt therapy to the tumor microenvironment (TME) of the patient among the numerous options of monoclonal antibodies or small molecules. Predicting the best combinatorial regimen remains an unmet medical need. Here, we report a multiplex functional and dynamic immuno‐assay based on the capacity of the TME to respond to ex vivo stimulation with twelve immunomodulators including immune checkpoint inhibitors (ICI) in 43 human primary tumors. This "in sitro" (in situ/in vitro) assay has the potential to predict unresponsiveness to anti‐PD‐1 mAbs, and to detect the most appropriate and personalized combinatorial regimen. Prospective clinical trials are awaited to validate this in sitro assay.
To predict cancer resistance to PD‐1 blockade and design suitable combinations of immunomodulators, a 60‐h functional in sitro assay was set up in 43 tumors that allowed calculation of the “Immune Reactivity Score (IRS)” based on 17 TCR‐dependent‐ cytokines/chemokines.

The paper explained
Predicting primary resistance to PD‐1 blockade and adapting combinatorial regimens in a stratified or personalized manner remain problematic in cancer treatment. Diagnosis tools for decision making are urgently needed in cancer patients.
We set up a functional dynamic multiplexed immunophenotyping assay, measuring up to 50 parameters after 60 h of ex vivo stimulation with 12 immunomodulators. This flow cytometry‐ and Luminex‐based assay was performed in 43 fresh tumors. We selected a 17 analyte‐based immune reactivity score that detected primary resistance to PD‐1 blockade. 26% of tumors exhibited both anergic tumor infiltrating lymphocytes (TILs) to rIL‐2 and no responses to PD‐1 blockade. The lack of CXCL10 release from fresh neoplasia was associated with primary resistance to PD‐1 blockade. In seven cases amenable to in vivo therapy with PD‐1 blockade, this “in sitro” assay anticipated the resistance to therapy in five tumors. 50% of primary resistance to PD‐1 blockade could be shifted toward immunoreactivity using personalized combinatorial regimens. The presence of a specific regulatory T‐cell subset correlated with anti‐PD‐1 antibody‐induced immunosuppression that could be rescued by anti‐killer inhibitory receptor mAbs.
Albeit exemplified in only 43 cases in this report, the in sitro assay has the power to predict primary resistance to PD‐1 blockade and can propose a personalized combinatorial regimen of immunomodulators in 60 h based on freshly dissociated tumor specimen and a 17 analyte‐based score, advocating for its future validation in prospective clinical trials.
While immunotherapy has made great strides as a standalone and combined with conventional cytotoxic strategies, its effect is limited across tumor types and patient subsets (Topalian, 2015; Kalbasi & Ribas, 2020). The recent characterizations of multiple immune resistance mechanisms have fueled the development of novel agents to circumvent such limitations (Williams et al, 2020). Yet, the ability to predict and best overcome tumor resistance is not currently possible (Kalbasi & Ribas, 2020). A promising approach to circumvent primary resistance to programmed cell death‐1 (PD‐1) blockade is to target new immune inhibitory or agonistic checkpoints (Kalbasi & Ribas, 2020). In the near future, the use of combination strategies will increase the number of patients who are likely to benefit from immunotherapy (Riaz et al, 2017). However, several critical issues have yet to be addressed. First, the development and validation of predictive immune biomarkers are needed to guide immuno‐oncology (I‐O) treatment decisions across various malignancies. Secondly, the rapid diagnosis and rationale lending support to personalized combinatorial regimens will require a formalized scientific and clinical framework. Hence, it remains to be seen whether the future of I‐O will rely on patient stratification or personalization.
Accumulating evidence highlight the capacity of anti‐PD‐1/PDL‐1 monoclonal antibodies (mAbs) to target tumor infiltrating lymphocytes (TILs) in situ within tumor beds (Wei et al, 2018). Tertiary lymphoid organs (Thommen et al, 2018), temporal and metabolic changes in T‐cell clones according to regional nonsynonymous tumor mutations (Inoue et al, 2016; Riaz et al, 2017; Joshi et al, 2019), and the efficacy differences between adjuvant and neoadjuvant settings (Liu et al, 2016) support the critical impact of the tumor microenvironment (TME) at the start of I‐O to dictate the early outcome at 6–8 weeks first CT scan. Therefore, technical approaches directly assessing the dynamic functionality of immune checkpoint inhibitors on the native TME of accessible tumors may be instrumental to accelerate decision making in clinical management.
To do so, we developed a dynamic system biology approach aimed at defining key patient immunometrics. These metrics outlined relevant “in situ” prognostications of patient response through “ex vivo” reactivity of melanoma to cytotoxic T‐lymphocyte‐associated protein 4 (CTLA4) blockade (Jacquelot et al, 2017). In extending this high content screening to various histological types of primary tumors amenable to PD‐1 blockade, we refined this in sitro assay using an immunoreactivity scoring of 17 selected soluble parameters to best assess the functional potential of immune infiltrates to twelve immunomodulators combined to anti‐PD‐1 mAbs. This in vitro/in situ (“in sitro”) assay could identify surrogate markers of immune reactivity and had the potential to predict in vivo responses to anti‐PD‐1 mAbs.
Our population consisted of 43 patients with resectable and analyzable tumors (NSCLC [L, n = 16], kidney [K, n = 20], head and neck [HN, n = 4], ovarian [O, n = 1], and urothelial carcinoma [B, n = 2]) with 41/43 being naive untreated patients benefiting from a surgery in various Paris hospitals (refer to patients characteristics in Appendix Table S1). Among tumors > 2 cm in size (n = ~ 120) emanating from the operating room, we processed 43 tumor samples that met our internal eligible criteria for in sitro assays (cutoff value for alive CD45+ cells: > 0.2% corresponding to 10–20 and 100–200/tumor infiltrated lymphocyte (TIL) mm2 within tumor nests and stroma, respectively (Fig EV1A), and absolute cell number > 1 million; Appendix Tables S2 and S3). Of the tumor samples available for immunophenotyping using 90 parameter‐based flow cytometry at D0 (n = 34), CD45− tumor/stromal cells represented 23.9 ± 3.7% of the TME. The phenotype of CD45+ leukocytes comprising 10 cell types is comprehensively presented in Appendix Table S1–S3 and Appendix Figs S1 and S2.

TCR‐dependent soluble factors (SF) and correlations with immune effector functions after PD‐1 blockade
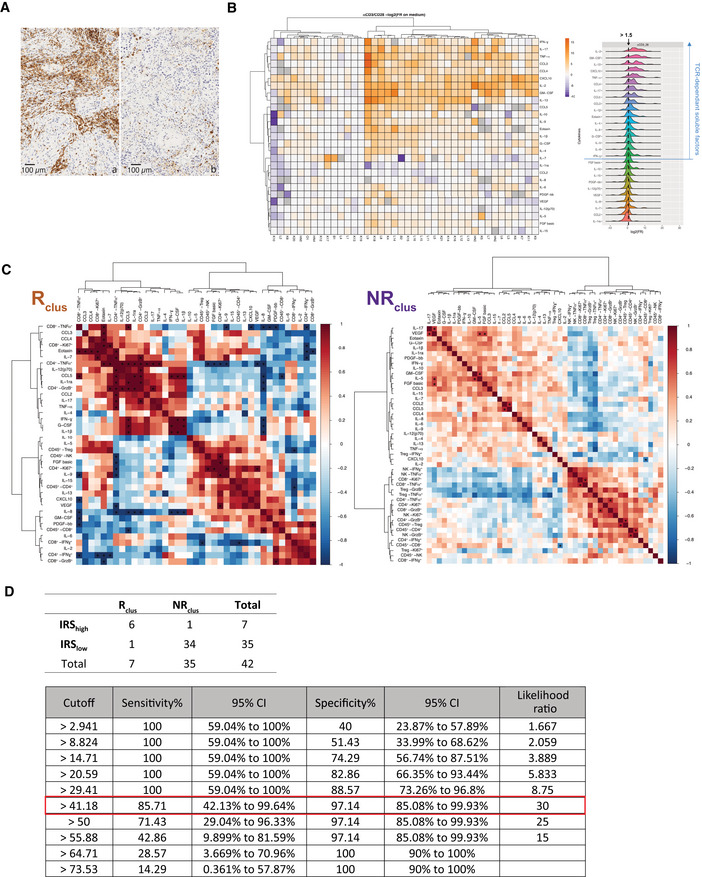
Representative micrograph pictures of TIL densities in stroma surrounding the tumor or tumor nests in two cases containing high (15%, (A)) or low (0.7%, (B)) CD45+ TILs in a surgical specimen. Scale bar representing 100 µm is indicated on the picture.
Left panel: Heatmap of the non‐supervised hierarchical clustering using 27 SFs, segregating patterns of immune reactivity of the TME (n = 42) following a 60‐h stimulation with anti‐CD3 and anti‐CD28 mAbs (TCR cross‐linking). The heatmap shows z score‐normalized concentration of soluble factors. Each column represents a tumor and each row a SF. Fold ratio of SF concentrations after TCR cross‐linking over the concentrations in untreated cells (medium) were log2 transformed. Similar data were obtained using isotype control mAbs instead of medium (Appendix Fig S2). The color gradient from purple up to orange indicates increasing gradients of concentrations. Missing values are shown in gray. Both rows and columns are clustered using correlation distance and average linkage. Right panel: distribution of fold ratio of each SF following TCR cross‐linking.
Spearman correlation matrices of SFs and FACS‐based effector functions post‐PD‐1 blockade (fold ratio over medium) for Rclus and NRclus tumors according to the clustering of Fig 1B. For each tumor sample, only FACS‐based effector functions with data ≥ 500 events in are represented here. *P values < 0.05.
Assessment of the concordance of the clustering score (Rclus and NRclus) and the immune responsive score (IRSlow and IRShigh; above) and corresponding sensitivity and sensibility values of the IRS for the 42 patients (below). The best cutoff value with the highest likelihood ratio is framed in red.
Source data are available online for this figure.
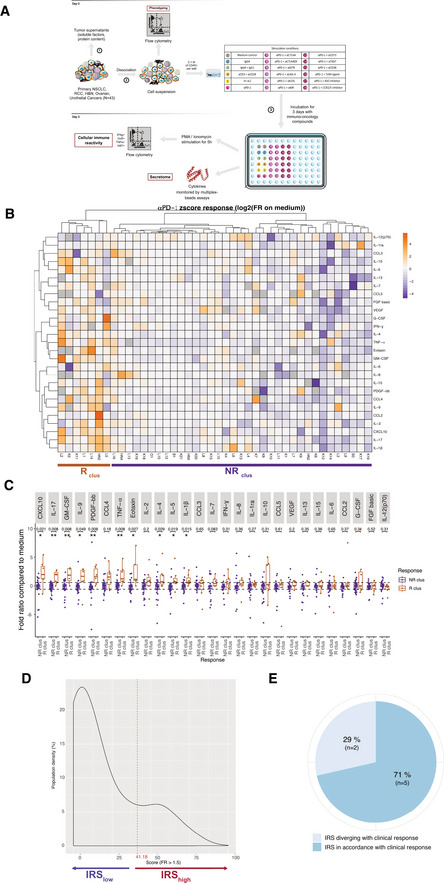
We next analyzed the dynamics of the TILs within their native, although dissociated, TME after 3 days of in sitro stimulation with anti‐PD‐1 mAbs through the investigation of conventional effector lymphocyte functions, regulatory T cell (Treg) cells (CD25hiFoxp3+CD4+) and secretory patterns of the mixture (Fig 1A, Appendix Table S1–S3). Following stimulation with anti‐PD‐1 mAbs, and normalization onto medium values to classify tumor responsiveness (medium values being mostly equivalent to isotype control mAbs values [Appendix Fig S3]), we used a non‐supervised hierarchical clustering of z score‐normalized concentrations of multiple (n = 27) immune and non‐immune soluble factors (SFs) monitored by beads‐based multiplex assay. The heatmap of this clustering highlights two categories of TME. Approximately, 17% (7/42) (4 L, 2 K, 1 HN) of tumors exhibited increased levels of most analytes above the mean of the whole cohort after stimulation with anti‐PD‐1 mAbs (called henceforth “Rclus”, Fig 1B). The most significant differences between tumors responding (Rclus) or not responding (NRclus) to anti‐PD‐1 mAbs resided in the release of CXCL10, GM‐CSF, PDGF‐bb, eotaxin, and IL‐5; as well as inflammatory cytokines (IL‐1β, tumor necrosis factor [TNF]α, IL‐17; Fig 1C) and not the usual Th1 cytokines. Most of these immunometrics were compatible with the prominent soluble mediators secreted after T‐cell receptor (TCR) cross‐linking (Fig EV1B). In Rclus, the concentrations of the 27 cytokines/chemokines after 60 h of anti‐PD‐1 mAbs correlated with the percentages of CD8+ T cells within CD45+ leukocytes, as well as the effector functions of the immune infiltrate (Ki67, TNFα, interferon [IFN]γ, granzyme B [GrzB]; Fig EV1C, left panel). In NRclus tumors, however, the Th1 chemokine CXCL10 exhibited inverse correlation with the proportion of CD8+ T cells (Fig EV1C, right panel). Of note, the integration of all 39 immunometrics did not improve the clustering. To refine the classifier, we attributed individual scores based exclusively on TCR‐dependent SFs. They were defined as analytes for which the fold ratio between unstimulated and anti‐CD3/anti‐CD28 mAbs‐stimulated tumors (concentration anti‐CD3/anti‐CD28/concentration medium) was superior to 1.5 (Fig EV1B, right panel). The “immune reactivity score” (IRS) assigned +1 to each of the 17 TCR‐dependent SFs reaching ≥ 1.5‐fold ratio following PD‐1 blockade (concentration anti‐PD‐1/concentration medium) and integrated the sum of these 17 parameters (transformed in a percent value). Tumors accrual in IRS is depicted in Fig 1D and detailed in Appendix Table S4. "Immune reactive" status was defined by the cutoff of IRS ≥ 41.18 which was determined to maximize the sensibility and specificity for the best concordance with the hierarchical clustering classifier (Fig EV1D). This means that patients classified as IRShigh have ≥ 7 out of 17 parameters that are increased by greater than or equal to 1.5‐fold ratio. 7/42 (17%) of the tumor samples fell into this category including 5 L, 1 K, and 1 HN cancers. As expected, most of them corresponded to the specimens considered “Rclus” in the non‐supervised hierarchical clustering method. Given the expected clinical objective response rate obtained with systemic administration of anti‐PD‐1 mAbs across malignancies, we surmised that the in sitro IRS may be a valuable tool to evaluate the likelihood of a patient to respond to PD‐1 blockade. "In vivo veritas" could then be prospectively validated by assessing the definitive clinical response of six of our patients (L3, L6, L8, K1, K7, and K11) for seven in sitro assays and evaluations in the course of anti‐PD‐1 ± anti‐CTLA4 mAbs administration for disease progression. In 5/7 assays, the in sitro IRS aligned with the clinical outcome (Fig 1E, Appendix Table S5). One patient enrolled in the TITAN study (K11) started with 8 weeks on anti‐PD‐1 treatment. Because of disease stability, K11 was switched to the combination of anti‐PD‐1 + anti‐CTLA4. This patient demonstrated an improved response to combination checkpoint blockade following single line PD‐1 blockade. For K11, the IRS was capable of predicting the response to both anti‐PD‐1 alone and combinatorial checkpoint blockade (detailed thereafter in Fig 3, Appendix Table S5). However, in one case where the IRS did not correspond to the clinical response (L8), we noticed that, following primary tumor resection, the patient benefited from local irradiation on a distant lesion concomitant to PD‐1 blockade. It is possible that the local irradiation may have stimulated an abscopal response, suggesting that the IRS should have been evaluated post‐irradiation in the lesion exposed to X‐rays. Consequently, the in sitro platform analyzing 39 immunometrics allowed the a priori segregation of tumors in anti‐PD‐1 R or NR tumors using two converging methods taking into account 17 soluble analytes, that correlated with effector functions of TILs only in R tumors. Higher sample size is required to improve the statistical power of this prediction prospectively.

Clustering of the TME secretory pattern based on the in sitro platform to stratify response or resistance to PD‐1 blockade
Overview of the in sitro diagnosis platform.
Heatmap of the non‐supervised hierarchical clustering (n = 42) using 27 soluble factors (SF), secreted after 60 h‐PD‐1 blockade. Missing values are shown in gray. Both rows and columns are clustered using correlation distance and average linkage.
Fold ratios and ranges between Rclus and NRclus for each SF. Box plots display group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers). Wilcoxon rank‐sum test and P values with a Benjamini–Hochberg (BH) correction procedure (*P < 0.05, **P < 0.01) are indicated for each SF.
Density of patients according to the immune reactivity score (IRS), with threshold of positivity at 41.18 is indicated in dashed line.
In vivo veritas "validation" of the in sitro platform on seven available clinical data sets.
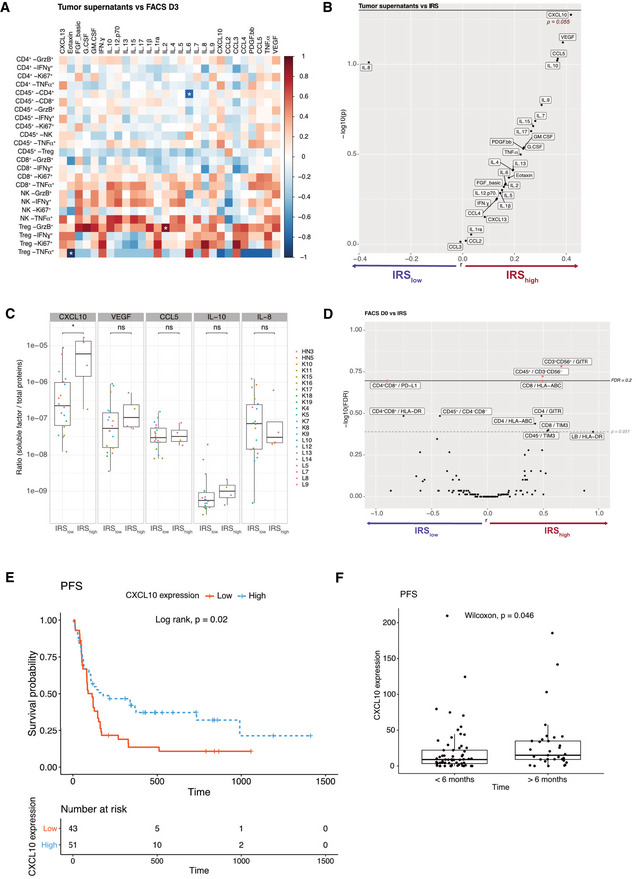
We next considered SFs that are spontaneously released immediately after surgery contained in the transport medium prior to being processed in the laboratory, henceforth referred to as “tumor supernatants” (Fig 1A). No meaningful correlations were observed between SFs from tumor supernatants and their TIL phenotypes after PD‐1 blockade (60 h; Fig 2A). We next analyzed potential links between such SFs and the IRS (< or > 41.18). Only one chemokine, the Th1‐associated CXCL10, significantly correlated with the response to anti‐PD‐1 mAbs (IRS > 41.18; Fig 2B and C). Vascular endothelial growth factor tended to positively predict response to PD‐1 blockade, possibly reflecting tumor lymphangiogenesis and tertiary lymphoid organogenesis (Fankhauser et al, 2017). In contrast, IL‐8 tended to correlate with resistance to PD‐1 blockade, as recently reported (Schalper et al, 2020). We next examined correlations between the IRS and the fluorescence‐assisted cell sorting (FACS)‐based TIL phenotypes at diagnosis (D0; Figs EV2, EV3). This approach highlighted two potential predictors of response to PD‐1 blockade: the expression of glucocorticoid‐induced TNFR‐related protein (GITR) on CD3+ CD56+ T cells (Figs 2D and EV2G) and the content in CD3−CD56− cells (Figs 2D and EV2A). However, membrane PD‐1 ligand (PD‐L1) on CD4+ CD8+ T cells was associated with resistance to PD‐1 blockade, as already reported (Jacquelot et al, 2017) (Fig 2D and EV3).

Biomarkers associated with response to in sitro PD‐1 blockade
ASpearman correlation matrix between concentrations of SF in tumor supernatants and FACS‐based immune effector functions at 60 h post‐PD‐1 blockade (in fold ratio over medium alone) for n = 43 tumors. *P < 0.05.
B–DVolcano plot of IRS (IRS > 41.2 underlined in red) and the concentrations of SF for 43 tumors (B) or phenotype of TILs (D) at baseline (CXCL10; P = 0.055) of log10‐transformed Wilcoxon rank‐sum test P values with a Benjamini–Hochberg (BH) correction procedure (FDR) or not (P) and the log10‐transformed ratio according to the IRS. Significant biomarkers are filled in red (FDR < 0.2) and associated biomarkers (P < 0.051) are highlighted. (C) Detailed bar graph of the concentrations of SF in (IRShigh > 41.2, n = 4) and (IRSlow, n = 18) tumors. Box plots display group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers). Statistical analyses: Wilcoxon rank‐sum test, ns. P > 0.05, *P < 0.05.
E, F In vivo validation of the predictive value of tumor CXCL10 for the response to PD‐1 blockade in NSCLC patients. Kaplan–Meier progression‐free survival (PFS) curves according to the median value (E) or cutoff value (< 6 months, n = 61; > 6 months, n = 32) (F) of tumor CXCL10 relative expression from two independent cohorts of NSCLC patients. (Appendix Table S6).
Source data are available online for this figure.

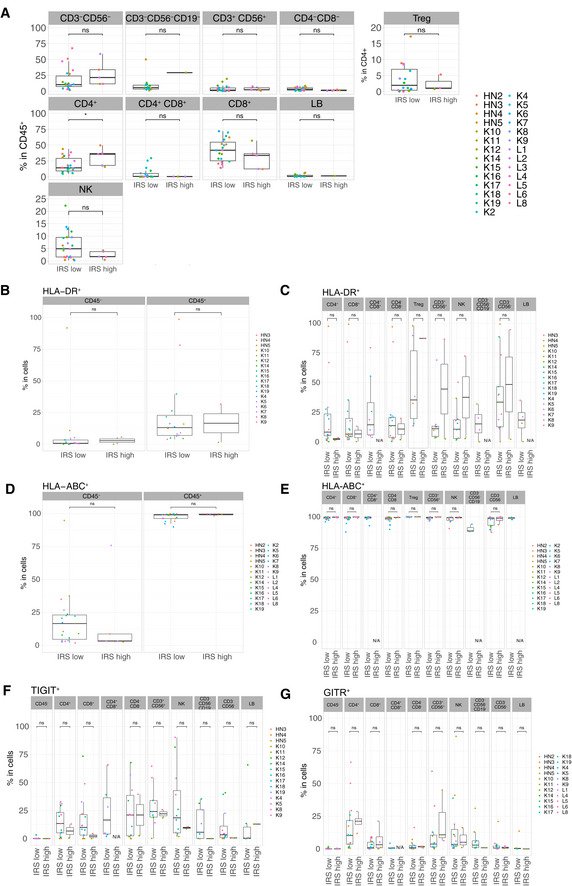
Differential cell surface expressions of activation and exhaustion markers in IRShigh vs IRSlow tumor samples
A–GFlow cytometry determination of various cell surface markers (as indicated) within CD45− cells or different tumor immune subsets among CD45+ cells between the two groups of tumors (IRShigh vs IRSlow), according to the clustering depicted in Fig 1D. Box plots display group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers). In each box plots, each dot represents one tumor. Statistical analyses: Wilcoxon rank‐sum test, ns. P > 0.05, *P < 0.05. Only data ≥ 500 events were plotted here. N/A: data not available or < 500 events.

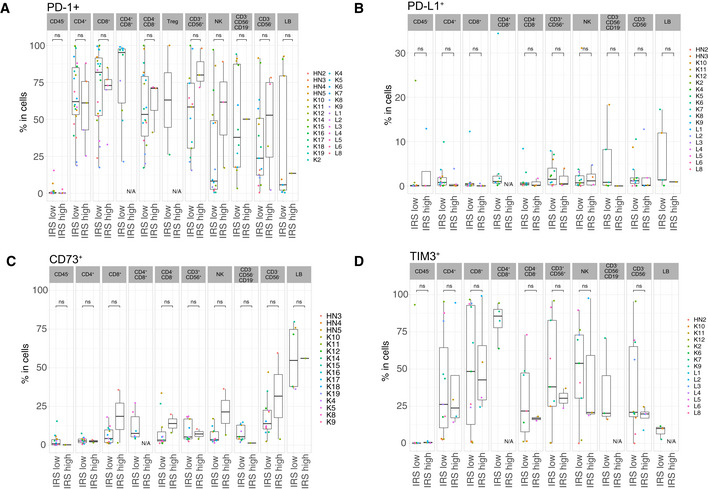
Differential cell surface expression of PD‐L1, PD‐1, CD73 and TIM3 in IRShigh vs IRSlow tumor samples
A–DFlow cytometry determination of various cell surface markers (as indicated) within different tumor immune subsets or CD45‐ cells between the two groups of tumors (IRShigh vs IRSlow), according to the clustering depicted in Fig 1D. Box plots display group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers). In each bar graph, each dot represents one tumor. Statistical analyses: Wilcoxon rank‐sum test, ns. P > 0.05. Only data ≥ 500 events were plotted here. N/A: data not available or < 500 events.
Finally, in order to validate the only significant marker that the in sitro platform highlighted, we retrospectively analyzed the predictive value of tumor CXCL10 expression (evaluated by RNA‐seq on tumor biopsies at diagnosis) for the response to PD‐1 blockade in two independent cohorts of L cancer patients (N = 94 in total) who had a follow‐up > 6 months after PD‐1 blockade, considering progression‐free survival as a continuous variable or a cutoff at 6 months. Indeed, tumoral CXCL10 expression at diagnosis was significantly associated with prolonged PFS in univariate analysis (Appendix Table S6, Fig 2E and F).
Altogether, the in sitro immunodynamic analysis allowed us to re‐enforce previously reported biomarkers, such as the good and bad prognostic value of CXCL10 (Choueiri et al, 2016), IL‐8 (Schalper et al, 2020), and PDL‐1 on double‐positive CD4+ CD8+ T cells (Jacquelot et al, 2017; Menard et al, 2018), supporting the rationale of using this accelerated approach in clinical decision making.
Next, we addressed whether this in sitro assay would reveal if tumors were susceptible to immune reactivity with PD‐1 blockade alone or combined with other I‐O compounds. Each of these compounds was used at the saturation dosing. Bearing in mind that sample number per combination test are different, out of seven IRShigh samples (IRS > 41.18), 4 exhibited a slightly improved IRS adding either anti‐CTLA4 (K11, Fig 3A–C), anti‐CD73 (L16, Fig 3A and D), anti‐GITR (K11, HN3, Fig 3A), or IDOi (L1, Fig 3A). Interestingly, the defucosylated Fc portion of anti‐CTLA4 mAb, expected to increase antibody‐dependent cell cytotoxicity and removal of Treg (Arce Vargas et al, 2018) did not improve the immune status of the tumors over the native compound (Fig 3A–C). When turning to tumors that failed to exhibit a response to anti‐PD‐1 mAbs in sitro (IRS < 41.18), we first analyzed those that were also non‐responders to recombinant IL‐2 (rIL‐2; N = 19/27; Appendix Table S7). Tumors anergic to rIL‐2 exhibited higher basal expression of PD‐1 or PDL‐1 on T, natural killer (NK), B, and myeloid cells (Appendix Fig S4A). Among these, 26.3% (5/19) anergic TME could be rescued with an anti‐PD‐1 mAb‐based combinatorial regimen. Interestingly, of the 8 tumors exhibiting an anti‐PD‐1 IRS < 41.18 but an rIL‐2 IRS of ≥ 41.18, 6/7 responded to at least one combinatorial regimen and one could not be tested with other compounds. Considering all tumors harboring an IRS < 41.18, and tested for combinations specified, 50% (13/26) could be rescued by at least one anti‐PD‐1 mAb‐based combination (Fig 3E). Not all combinations were tested in the 26 tumors (refer to Fig 3E). In a rare case (K18), combination with any tested compounds, except anti‐CTLA4, was effective (Fig 3F and G, left panel), while L12 (Fig 3F and G, right panel) required the addition of Toll‐like receptor 4 (TLR4) agonist. There was no correlation in our assay between the cell surface expression of the target molecules tested in tumors at baseline and the immune reactivity to each targeting mAbs (IRS) and any respective combinatorial regimen (Appendix Fig S4).
Altogether, the in sitro assay indicated that 50% of IRSlow to anti‐PD‐1 mAbs could be rescued by a combination. However, optimal responses harbored a variegated profile, suggesting that personalization as opposed to stratification may in fact be the preferred solution to circumvent primary resistance to PD‐1 blockade (Fig 3E, lower line). Additional studies to increase the sample size for each combination are needed for robust determination of therapeutic complementarity in this system.

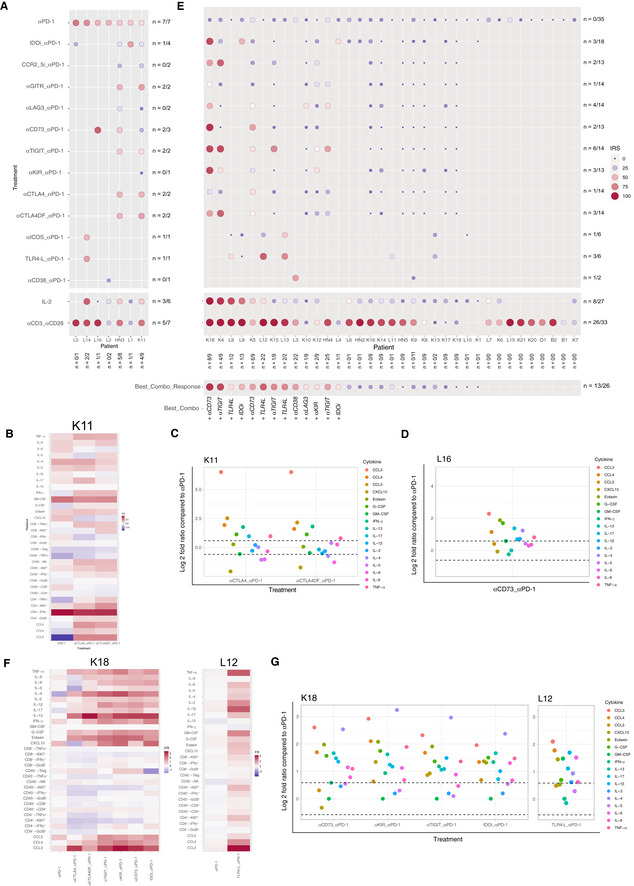
Reactivating anergic TME with anti‐PD‐1 mAb‐based combinatorial regimen
A–G(A, E) The IRS was determined for each tumor after PD‐1 blockade alone (top line), or combined with immunomodulators in two groups of tumors (IRSanti‐PD‐1> (A) or < 41.18 (E)). The size and color of the bullet both correspond to the IRS. The “n” corresponds to the number of immune reactive tumors for each combination (horizontally) and to the number of combinations that induced a positive immune reactivity (≥ 41.18) per tumor (vertically). Best corresponding combination responses are indicated below for each patient. Note that these experiments do not allow to establish direct comparisons of relative efficacy in‐between each compound, given the limited amount of samples tested, the lack of dose ranges tested for each compound and/or sample availability. (B–D, F, G) Focus on four cases for the reactivity to anti‐PD‐1 mAbs alone or combined with immune checkpoints. Heatmap depicting the fold ratio for each immunometrics between stimulation with mAbs vs medium and raw data illustrating the increase of the soluble factors (SFs) of the combinations compared to anti‐PD‐1 alone.
Cancer hyper‐progression during the first four courses of systemic anti‐PD‐1 mAbs remains a potential concern (Champiat et al, 2018). Intrigued by a drop in cytokine release profile in some tumors (Fig 1B), not explained by activation‐induced cell death of lymphocytes or increased proliferation of tumor cells, we designed a score of hyporeactivity for the 27 SFs of the multiplex array, meaning a diminution by 10 of the fold ratio (FR < 0.1) between anti‐PD‐1 stimulated vs non stimulated TILs, affecting +1 for each SFs and the sum of them for the hypo‐responsive score (HRS). The median of the r was 5.55 (Fig EV4A and B) and 6 tumors presented a HRS > 5.55 (Appendix Table S8). The only predictive factor associated with HRShigh was the co‐expression of CTLA4 and C‐C chemokine receptor 5 (CCR5) in tumor Treg (Fig EV4C and D), as already described (Kamada et al, 2019). Elimination of Tregs by FACS‐cell sorting allowed for increased cytokine release, while adding them back into the coculture prevented it (Fig EV4E). Moreover, anti‐Killer cell immunoglobulin‐like receptor (KIR) mAbs was the best condition to prevent anti‐PD‐1 mAbs‐induced HRS > 5.55 (Fig EV4F, Appendix Table S8). Thus, the in sitro platform may be able to detect a hypo‐responsive TME, based on three criteria: (i) an elevated HRS (> 5.55) following PD‐1 blockade, (ii) the presence of a particular Treg subset, and (iii) the efficacy of anti‐KIR mAb in reducing the HRS under its threshold. This interesting result deserves prospective validation in clinical trials.

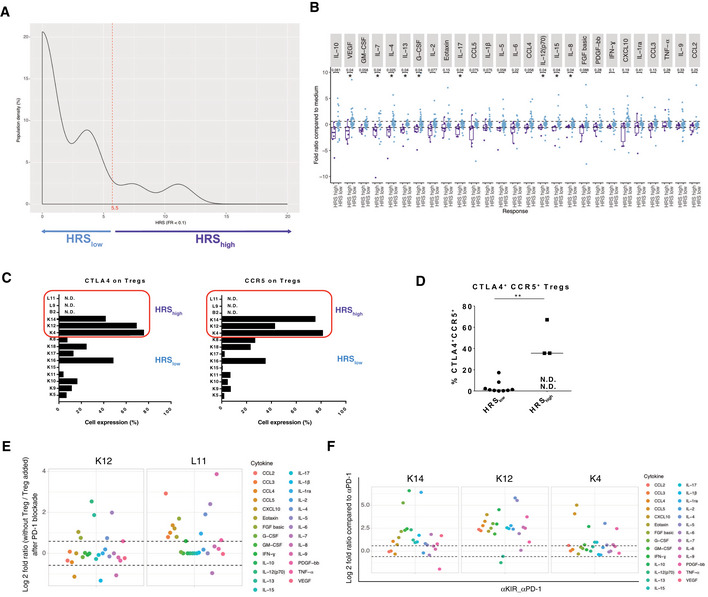
Hypo‐responding tumors with anti‐PD‐1 mAbs
Density of patients for each hypo‐responsive score (HRS) of the whole tumor cohort. The HRS was calculated taking into account all the 27 SFs. A tumor was considered "hypo‐responding" (or HRShigh) when the HRS ≥ 5.5, as underlined in light violet.
Bar graph according to the fold ratio range between HRShigh (> 5.5) and HRSlow (< 5.5). Box plots display group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers). Each dot represents one tumor for each SF. Statistical analyses: Wilcoxon rank‐sum test and P values with a Benjamini–Hochberg (BH) correction procedure (*P < 0.05) are indicated for each SF to interpret the significance between HRShigh vs HRSlow groups of tumors.
Detailed CTLA4 and CCR5 membrane expression levels (percentage) on each of the 12 (available) tumors evaluated at RT. N.D.: measure could not be performed.
Flow cytometric dot plot analysis of the percentages of Treg co‐expressing CCR5 and CTLA4 on their surface expression in the immune infiltrate after dissociation in 12 (available) cases. Black line represents the mean of the group. Statistical analyses: Wilcoxon rank‐sum test, **P < 0.01. N.D.: not done.
In sitro assay with or without Treg. Same experimental setting was performed as the one described in Fig 1A after cell sorting of CD25+PD‐1+ Treg from TILS, alone (without Treg), or restored with Treg cells at a 10:1 ratio E:Treg ratio (Treg added), then stimulated with anti‐PD‐1 mAbs. Upper and lower dashed line represent a 1.5‐fold increase and decrease, respectively, in soluble factor release.
Efficacy of anti‐KIR mAbs in preventing hypo‐responsiveness to PD‐1 blockade for K14, K12 and K4. All soluble factors (SF), i.e., HRS components, in anti‐PD‐1 + anti‐KIR mAbs were compared to anti‐PD‐1 mAbs. Upper and lower dashed line represent a 1.5‐fold increase and decrease, respectively, in soluble factor release.
Source data are available online for this figure.
Finally, our initial attempt to scale down the 17 plex‐based in sitro platform, from a whole tumor to a large biopsy, was not a major technical challenge. Hence, prospective clinical trials are warranted to validate these results to develop a platform as decision aid tool for future I.O.
Patients over 18 years old from Gustave Roussy Cancer Campus, Marie Lannelongue, Cochin, Tenon, Foch, Kremlin‐Bicêtre, and Saint Joseph hospitals, with stage I/II/III lung (L, n = 16), kidney (K, n = 20), head and neck (HN, n = 4), ovarian (O, n = 1), and bladder carcinoma (B, n = 2) primary resectable tumors provided written informed consent according with protocols reviewed and approved by institutional ethics committee including the investigator‐sponsored, study “mAb in sitro test”, N°ID‐RCB: 2016‐A00732‐49. The experiments conformed to the principles set out in the WMA Declaration of Helsinki and the Department of Health and Human Services Belmont Report.
4 µm‐thick sections were prepared from tissue samples fixed in buffered formalin pH 7.4 (Merck, Darmstadt, Germany), embedded in paraffin wax (Sakura, Alphen, The Netherlands), and cut with a microtome (Leica, Wetzlar, Germany). One section was stained with hematoxylin–eosin and used for the evaluation of TILs, which was performed according to international recommendations (Hendry et al, 2017). One section was used for CD45 immunodetection. Briefly, an indirect immunoperoxidase technique was applied to deparaffinized sections. A combination of two CD45 mouse mAbs, diluted 1:200, was used (2B11 + P7/26; Dako, Glostrup, DK). The reaction was performed with an automated stainer (Bond RX, Leica, Wetzlar, Germany). The density of CD45+ cells was evaluated within the tumor tissue by a senior pathologist; labeled cells were counted visually in at least 10 high power fields of 1 mm2 each; the result was expressed as the mean cell number/mm2.
Resected pieces were kept in NaCl or RPMI 1640 (GIBCO Life Technologies, ref: 31870‐025) for 6–18 h prior to dissociation. After 5 min at 425 g centrifugation, supernatants, called “tumor supernatants”, were frozen at −80°C until their use. These supernatants were controlled and normalized for total proteins concentration. To do this protein calibration, 1 µl of tumor supernatants was tested using Micro BCA™ Protein Assay Kit (Thermo Fisher, ref: 23235) following manufacturer's protocol; and 50 µl of tumor supernatants were used for bead‐based multiplex immunoassays (Luminex™ technology) following manufacturer's instructions. SFs were then normalized by the total proteins concentration.
Resected cancer specimens from 43 patients were cut and placed in dissociation medium, which consisted of RPMI 1640 (GIBCO Life Technologies, ref: 31870‐025), Collagenase IV (50 IU/ml; Sigma‐Aldrich, ref: C2139), Hyaluronidase (280 IU/ml; Sigma‐Aldrich, ref: H6254), and DNAse I (30 IU/ml; Sigma‐Aldrich, ref: 260913), and run on a gentle MACS OctoDissociator (Miltenyi Biotec). Dissociation time lasted 1 h under mechanical rotation and heating. Cell samples were diluted in PBS, passed through a cell strainer, and centrifuged for 5 min at 1,500 rpm. Cells were finally resuspended in PBS, counted with Precision Count Beads™ (Biolegend, ref: 424902) by flow cytometry following manufacturer's protocol, then stained for flow cytometric analyses or resuspended in fetal calf serum containing 10% of dimethyl sulfoxide (DMSO; SIGMA, ref: 276855) for storage in liquid nitrogen.
Dissociated cells from K, L, HN, O, B tumors (66% freshly harvested and 34% from frozen in DMSO) were stained for D0 phenotyping (0.5–0.25 × 106 of CD45+ cells per panel) and incubated in 96‐well plate at 0.1 × 106 of CD45+ cells per well in complete medium (RPMI 1640 (GIBCO Life Technologies, ref: 31870‐025) supplemented with 10% human AB serum (Institute Jacques Boy, ref: 201021334), 1% Penicillin/Streptomycin (GIBCO Invitrogen, ref:15140‐122), 1% l‐glutamine (GIBCO Life Technologies, ref: 25030‐024) and 1% of sodium pyruvate (GIBCO Life Technologies, ref: 11360‐039)) and with isotype control, agonist or antagonist mAbs, or with small molecules as described in Fig 1A. After 60 h of incubation with or without drugs, supernatants were collected for bead‐based multiplex immunoassays (Luminex™ technology) and cells were stimulated with PMA (5 ng/ml; Sigma‐Aldrich, ref: 524400), ionomycin (125 ng/ml; Sigma, ref: 10634), brefeldin A (1 µl/ml; eBioscience, ref: 00‐4506‐51), and Golgi Stop (4 µl/6 ml; BD Biosciences, ref: 554724). After 5 h, cells were harvested and then labeled for membranous and intracellular molecules according to the manufacturer's protocol.
The cell suspension was stimulated for 60 h with the following reagents: anti‐PD‐1 (nivolumab [Bristol‐Myers Squibb (BMS)] and pembrolizumab [Merck], 10 µg/ml), isotypes (IgG4 or IgG1, 10 µg/ml), anti‐CD38 (daratumumab, Janssen‐Cilag, IgG1, 5 µg/ml), anti‐CD73 (BMS‐986179, BMS, IgG1, 10 µg/ml), anti‐CTLA4 (ipilimumab, BMS, IgG1, 10 µg/ml), anti‐CTLA4 defucosylated (CTLA4DF, BMS, IgG1, 10 µg/ml), anti‐GITR (BMS‐986156, BMS, IgG1, 10 µg/ml), anti‐inducible T‐cell co‐stimulator (GSK3359609, IgG4, GlaxoSmithKline (GSK), 10 µg/ml), anti‐KIR (BMS‐986015, BMS, IgG4, 10 µg/ml), anti‐lymphocyte‐activation gene 3 (LAG3; BMS‐986016, BMS, IgG4, 10 µg/ml), anti‐T‐cell immunoreceptor with Ig and ITIM domains (TIGIT; BMS‐986207, BMS, IgG1, 10 µg/ml), CCR2/CCR5 inhibitor (BMS‐6876814, BMS, 10 nM), indolamine 2,3‐dioxygenase inhibitor (INCB024360, Incyte, 5 mM; BMS‐986205, BMS, 125 ng/ml), TLR4 agonist (GSK1795091A, 10 µg/ml), anti‐CD3 (Thermo Fisher Scientific, clone OKT3, 10 µg/ml), anti‐CD28 (Thermo Fisher Scientific, clone CD28.2, 10 µg/ml), and rIL‐2 (PeproTech, ref: 200‐02‐11, 10 µg/ml). Each molecule was used at the saturating dosing according to manufacturer's recommendations.
For membranous labeling, TILs were stained to discriminate different lymphocyte subsets with fluorochrome‐coupled mAbs incubated for 15 min at room temperature (RT) and washed. Intracellular staining was performed after permeabilization with forkhead box P3 (FoxP3)/ Transcription Factor Staining Buffer Set (Thermo Fisher Scientific, ref: 00‐5523‐00) and intracellularly labeled with anti‐Foxp3‐APC (eBiosciences, clone PCH101) mAb at D0, or with anti‐ IFN‐γ‐PECy7 (BD Biosciences, clone 4S.B3), anti‐TNFα‐BV650 (BD Biosciences, clone MAb11), anti‐GrzB‐PECF594 (BD Biosciences, clone GB11) mAbs and Ki67 (BioLegend, ref: 350514 or BD Biosciences, ref: 556027) at D3, following the manufacturer's protocol. Cell samples were acquired on a BD LSRFortessa™ X‐20 flow cytometer (BD Biosciences) with single‐stained antibody‐capturing beads used for compensation (CompBeads, BD Biosciences, ref: 552843). Data were analyzed with Kaluza Analysis software v2.1 (Beckman Coulter). Of the tumor samples available for flow cytometry at D0 (n = 34), CD45− tumor/stromal cells represented 23.9 ± 3.7% of the TME. The CD45+ leukocyte composition, including T, B, NK, and myeloid cells were analyzed by flow cytometry in available specimens (Appendix Table S1–S3, Appendix Figs S1 and S2A and B). Based on the immunophenotyping of 20–90 parameters (10 cell types and 2–9 mAbs target molecules per patient), we found comparable and variable distributions of T, NK, B and myeloid cells across individuals and tumor types (Appendix Fig S2B). However, K carcinomas were the only cancer subtype we tested that presented more than 5% of CD4+ CD8+ cells (Appendix Fig S2B). Those CD4+CD8+ cells, rather CD4dimCD8bright, tended to express higher levels of human leukocyte antigen (HLA)‐DR, PD‐1, CD73, and T‐cell immunoglobulin and mucin domain‐containing protein 3 (TIM‐3) than their single positive CD4+ T or CD8+ T counterpart cells (Appendix Fig S2D, E, G and H), in accordance with previous work (Menard et al, 2018). Interestingly, while TILs from K tended to express more TIGIT than HN tumors, they also harbored significantly less CD73 on CD3−CD56− and NK cells (P < 0.05, P = 0.14, respectively), while presenting less HLA‐DR compared with HN cancers (Appendix Fig S2G–J). As expected, HLA‐ABC was less expressed in tumor cells than leukocytes (Appendix Fig S2C). Concurrently, CD4+ T, CD8+ T, and NK cells from L cancers seemed to express higher levels of GITR than in the other tumor types (Appendix Fig 2I). Of note, PD‐L1 was not broadly expressed on CD45+ or CD45− TME across these tumor types (Appendix Fig S2F).
Tumor supernatants were monitored using the Bio‐Plex Pro™ Human Chemokine BCA‐1/chemokine (C‐X‐C motif) ligand 13 set (Bio‐Rad, ref: 171BK12MR2) and the Bio‐Plex Pro™ Human Cytokine 27‐plex Assay (Bio‐Rad, ref: M500KCAF0Y). Supernatants from cultured cells at D3 were monitored using the Bio‐Plex Pro™ Human Cytokine 27‐plex Assay (Bio‐Rad, ref: M500KCAF0Y) according to the manufacturer's instructions. Acquisitions and analyses were performed on a Bio‐Plex 200 system (Bio‐Rad) and a Bio‐Plex Manager 6.1 Software (Bio‐Rad), respectively.
The immune reactivity score (IRS) was calculated taking into account the 17 TCR‐dependent SFs (those reaching a median of the fold ratio following TCR cross‐linking [concentration aCD3/aCD28/concentration medium] > 1.5 [refer to Fig EV1A]). We assigned +1 to each TCR‐dependent SF reaching > 1.5‐fold ratio after stimulation with anti‐PD‐1 mAbs (concentration anti‐PD‐1/concentration medium). The IRS corresponds to the sum of the positive SFs transformed in a percent value. A tumor was considered “immune reactive” (or IRShigh) when the immune reactivity score IRS ≥ 41.2. Table S3 summarizes each IRS for each patient tumor. The HRS was calculated taking into account all of the 27 SFs available. We assigned +1 to each SF reaching < 0.1‐fold ratio after stimulation with anti‐PD‐1 mAbs (concentration anti‐PD‐1/concentrationmedium). The HRS corresponds to the sum of all 27 parameters, establishing a median at 5.5 defining the HRShigh vs HRSlow. Figure EV4A summarizes each HRS for each patient tumor. Similar data were obtained using an isotype control mAb instead of medium (Appendix Fig S2).
Data representations were performed either with Prism 6 (GraphPad San Diego, CA, USA) or R v3.6 using tidyverse, dplyr, ggplot2, ggpubr, pheatmap, corrplot, ggdendro, Hmisc, or survminer packages. Box plots display a group of numerical data through their 3rd and 1st quartiles (box), mean (central band), minimum and maximum (whiskers), and each dot represents one tumor sample. All calculations and statistical tests were performed using R v3.6. Unless stated, P values are two‐sided and 95% confidence intervals for the reported statistic of interest. Individual data points representing the measurement from one tumor are systematically calculated from the corresponding distribution. Wilcoxon rank‐sum test was applied to assess differences in concentration between two different responses to treatment (R vs NR) or between different cell subtypes. When indicated, the false discovery rate (FDR, P > 0.2) was controlled using the Benjamini–Hochberg procedure. For the progression‐free survival (PFS) analysis, Cox regression model using survival R package was used to estimate hazard ratio (HR) of the explanatory variables and their 95% confidence intervals (CIs). Survival curve was estimated by Kaplan–Meier method, using the R package survminer. Optimal cutoff for CXCL10 expression was chosen based on a maximally selected rank statistics (Kamada et al, 2019). SFs and flow cytometry parameters fold ratios were calculated as log2 transformation of median values of stimulated vs unstimulated wells and were converted to z scores. Figure 1B has been generated with the R package Pheatmap. Hierarchical clustering of the 42 patients based on the z score of 27 SFs was performed using Euclidean distance and ward.D clustering. In Fig EV1C spearman correlation of SFs fold ratio (stimulated over unstimulated) clustering is performed using Euclidean distance and ward.D clustering. Spearman correlations are computed with the Hmisc R package. All P values and number of each groups are depicted in Appendix P value tables.
LZ designed and conducted the study, MB coordinated the ethical and experimental parts of the in sitro assay and interpreted data related to this work, AD, J‐EF, and A‐GG analyzed and interpreted data related to this work, AD, NV, CB, SL performed the in sitro experiments, NJ helped in the conception of the platform, J‐Y Scoazec performed IHC evaluation, DD and LR contributed to the statistical analyses, DB, SM and SS provided experimental and scientific help, AC provided scientific help, EB performed the CXCL10 RNA‐seq, BR and FG recruited patients for the CXCL10 RNA‐seq analysis, ST and LD collected clinical information, DJF, SY, JDW, MB, AH and TC provided I‐O compounds and scientific input, VTM, OC, CR, SF, BP, CG, IB, MR, CL, HB, MW, EF, IC, LA, YL helped in the recruitment and collection of the tumor specimen, FA, BG, J‐YS, GK and AM provided scientific input.
LZ received bench fees and signed research contracts with Tusk Therapeutics, GSK, BMS, Incyte and Transgene to screen their pipeline which helped performing this extensive study over the past 5 years. GSK authors are employees and stockholders of GSK. Other authors declare no conflict of interest.
UMR 1015 Immunologie des tumeurs et immunothérapie contre le cancer: https://www.gustaveroussy.fr/fr/umr1015
LZ and GK were supported by the Ligue contre le Cancer (équipe labelisée); Agence Nationale de la Recherche (ANR) francogermanique ANR‐19‐CE15‐0029, ANR Projects blancs; ANR under the frame of E‐Rare‐2, the ERA‐Net for Research on Rare Diseases; Association pour la recherche sur le cancer (ARC); Bristol‐Myers Squibb Company (International Immuno‐Oncology Network), Cancéropôle Ile‐de‐France; Chancellerie des universités de Paris (Legs Poix), Fondation pour la Recherche Médicale (FRM); a donation by Elior; the European Commission (ArtForce); the European Research Council (ERC); Fondation Carrefour; Institut National du Cancer (INCa); Inserm (HTE); Institut Universitaire de France; LeDucq Foundation; the LabEx Immuno‐Oncology; the RHU Torino Lumière (ANR‐16‐RHUS‐0008); H2020 ONCOBIOME, the Seerave Foundation; the SIRIC Stratified Oncology Cell DNA Repair and Tumor Immune Elimination (SOCRATE); FHU CARE, Dassault, and Badinter Philantropia, and the Paris Alliance of Cancer Research Institutes (PACRI). AC is supported by the CPRIT Research Training Program (RP170067). JEF was supported by Transgene and AGG was supported by FRM. AM has been or is currently an investigator in clinical trials sponsored by BMS, MSD, GSK/Tesaro, Janssen, Roche/Genentech, Pfizer, Astra Zeneca (AZ), Amgen. AM has been or is currently a member of Clinical Trial Scientific Steering Committee for AZ and GSK. AM has been or is currently a member of the scientific advisory board of the following companies: Merck Serono, Novartis, BMS, Symphogen, Amgen, Tesaro/GSK, Pfizer, Astra Zeneca/Medimmune, Servier, Sanofi. AM has provided Scientific & Medical Consulting to the following companies: Roche, Sanofi. AM is a member of the Data Safety and Monitoring Board for the following trial NCT02423863 (TLR3 agonist; Oncovir). AM has received research funding and or drug supply for pre‐Clinical and clinical research projects from: BMS, Boehringer Ingelheim, Idera, MSD, Fondation MSD Avenir, SIRIC (INCa‐DGOS‐Inserm_12551).
This study includes no data deposited in external repositories.