
Competing Interests: The authors have declared that no competing interests exist
‡ These authors share first authorship on this work.
Lower urinary tract symptoms (LUTS) result in morbidities; however, their association with the occurrence of hip fracture is relatively unknown in the context of Asian studies. The purpose of the study was to investigate this link with the hip fracture risk in Taiwanese men and women aged 50 years and above.
From 2000 through 2012, a population-based retrospective cohort study was conducted; claims data of 18,976 patients diagnosed with LUTS (dysuria, urinary retention, incontinence, and increased urinary frequency and urgency) were retrieved from Taiwan’s National Health Insurance Research Database. The patients were compared with 1:2 age, sex, and index year-matched controls (comparison group, n = 37,952). The incidence and hazard ratios of the hip fracture risk were calculated by the Cox proportional hazard regression models.
The mean age was 66.2 ± 9.7 years, and the proportion of men was 58.1% in both study groups. Fractures occurred in 772 patients and 1,156 control subjects. The corresponding incidences were 7.0 and 5.0/1000 person-years. Compared to the control subjects, the patients with LUTS had an increased hip fracture risk [adjusted hazard ratio (aHR) = 1.29; 95% confidence interval (CI): 1.17–1.42]. LUTS was independently associated with an increased hip fracture risk in both men (aHR = 1.24; 95% CI: 1.08–1.42) and women (aHR = 1.34; 95% CI: 1.18–1.53) (p for interaction = 0.557). Similarly, the subgroup effect of age on hip fracture risks was not found (p for interaction = 0.665).
The study found LUTS was associated with an increased risk of hip fracture. Large-scale prospective studies in diverse populations are required to investigate causalities.
The incidence of hip fractures increases with the rising aging population worldwide; consequently, society and the health care system experience major challenges because of significant disability, morbidity, and mortality [1–3]. Falls, osteoporosis, increased age, dementia, vision loss, and high body weight contribute to the hip fracture risk [4–8]. The incidence of osteoporosis rises with age; it frequently develops during menopause as bone fragility elevates the risk of, or results in fall-related hip fractures [9–11]. Hip fractures lead to increased hospital costs and possibly to secondary health problems or even death. Therefore, prevention of hip fractures and osteoporosis are imperative public health challenges.
Lower urinary tract symptoms (LUTS) are prevalent in elderly men (through benign prostatic hyperplasia) and women (due to menopause), characterized by incomplete voiding, hesitancy, and diminished stream and storage indications like urgency with incontinence, increased frequency, and nocturia. Significant morbidity [12–14] and a potential increase in the risk of falls may be observed; however, a significant connection is to reported. A systematic review of 15 studies stated an overactive bladder (OAB), nocturia, and anticholinergic medications were associated with an increased risk of falls and fracture; however, this was not concurred by the Osteoporotic Fractures in Men (MrOS) prospective cohort study [15–19]. Sporadic studies in Asian countries have compared this association. Studies in Korea have reported a link between LUTS and the risk of falls, possibly predisposing individuals to hip fractures; additionally, the employment of alpha-blockers for LUTS treatment was connected to an increased risk of hip fracture in elderly women [20, 21].
The present study aimed to investigate the association between LUTS and the risk of hip fracture in the elderly population of Taiwan.
The present population-based cohort study retrospectively analyzed data retrieved from Taiwan’s National Health Insurance Research Database. The National Health Insurance (NHI) comprises a single-payer mandatory-enrollment system established in 1995 [22]. It provides a comprehensive outpatient, inpatient, and emergency service coverage to >99% of the population contracted with 97% of hospitals and clinics across Taiwan. The Longitudinal Health Insurance Database (LHID) has been established for research purposes; it includes health records of 1 million individuals, with patient’s demographic data and medical claims randomly sampled in the 2000 registry of NHI beneficiaries. To ensure patient privacy and data security, all identifying information was encrypted by the National Health Research Institute. The Research Ethics Committee of the Hualien Tzu Chi Hospital approved the study (REC No: IRB 107-60C), and the need for informed consent was waived. The research was performed in accordance with relevant guidelines/regulations.
The patient selection process is detailed in Fig 1. The study population featured LUTS (exposed) and non-LUTS (comparison) cohorts included in the LHID between 2000 and 2012. Patients aged ≥ 50 years initially diagnosed with LUTS between 2000 and 2012, followed by two subsequent diagnoses within 1 year, were eligible for inclusion. The patients who did not receive 2 subsequent LUTS diagnoses within 1 year of their first diagnosis were excluded. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 788.1–788.4 and 788.63 were employed to identify patients with LUTS (dysuria, urinary retention, incontinence, and increased urinary frequency and urgency). The third diagnosis was utilized as the index date; follow-up began subsequently. The comparison group comprised a 1:2 age, sex, and index year-matched cohort. The index date was assigned the same as the matched LUTS cases. To ensure the inclusion of newly diagnosed cases, LUTS detected prior to 2000 and hip fracture evaluated before the index date were excluded from both study groups. Patients younger than the specified age limit were ruled out; hip fractures in such cases result from a high-impact trauma event. Additionally, < 2 subsequent diagnoses within 1 year of the initial detection were not considered in the study.

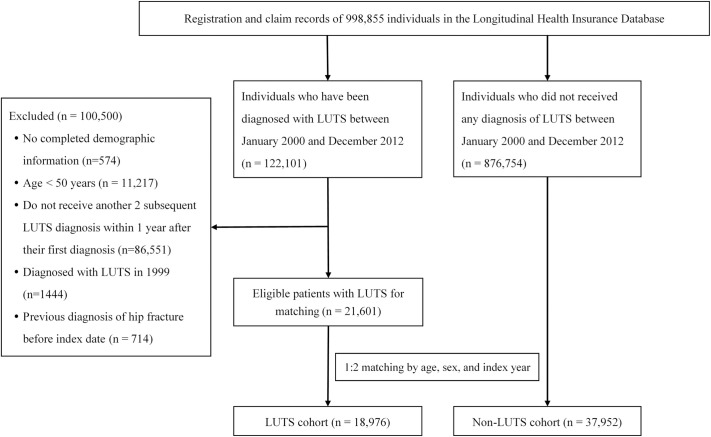
Study flow chart.
The primary outcome was the occurrence of hip fracture (ICD-9-CM codes 820.x and 733.14) during the follow-up. The accuracy of the diagnostic codes had previously been validated [23]. Patients were followed from the index date until the hip fracture, death, withdrawal from the LHID, or the final duration in the database (December 31, 2013). Additionally, the outcome was evaluated following stratification for age and sex.
Baseline patient characteristics considered to be potential confounders were identified by prescription codes, ICD-9-CM codes and procedures of the outpatient and inpatient reimbursement claims; pre-existing comorbidities included were diseases or conditions diagnosed in the year preceding the index date. The baseline medication included drugs prescribed for at least 30 days. The Charlson Comorbidity Index was calculated for each patient [24, 25]. The income was stratified by five levels in New Taiwan Dollars (NTD) as ≥60,000; 40,000−59,999; 20,000−39,999; 15,840−19,999; financially dependent, according to the income-related NHI premiums.
Statistical analysis was performed with Stata (version 13; Stata Corporation, College Station, TX, US). The distinction in the baseline characteristics between the groups was assessed considering the standardized mean difference, with a value < 0.1 considered negligible [26].
The cumulative incidence of the hip fracture was estimated by the Nelson-Aalen method from the initiation of the independent follow-up until the date of event occurrence or censoring. Therefore, the start of the follow-up time for each individual was reset from the calendar date to zero; the end was reset to the actual duration of the observed time. The between-group differences were compared by log-rank tests. The univariable and multivariable Cox proportional regression models were employed to calculate the hazard ratios (HRs) with adjusted values (aHRs), and 95% confidence intervals (CIs) for the hip fracture risk. One multivariable model was adjusted for all covariates listed in Table 1. A second model applied a forward model selection procedure using the score test method with p < 0.1 as the entry-level to include the baseline characteristics for adjustment. Age and sex-stratified sub-analyses were performed, and interaction tests were employed to determine the subgroup effects of age and sex on the hip fracture risk. All covariates listed in Table 1 were adjusted in the multivariable Cox proportional hazards regression model. Two-sided probability values of < 0.05 were considered statistically significant.

| LUTS | SMD | ||||
|---|---|---|---|---|---|
| Yes (n = 18,976) | No (n = 37,952) | ||||
| n | % | n | % | ||
| Age (years) | |||||
| 50–64 | 8,451 | 44.5 | 16,902 | 44.5 | 0.000 |
| 65–79 | 8,769 | 46.2 | 17,538 | 46.2 | 0.000 |
| ≥ 80 | 1,756 | 9.3 | 3,512 | 9.3 | 0.000 |
| Mean ± SD | 66.2 | ±9.7 | 66.2 | ±9.7 | 0.000 |
| Sex | |||||
| Male | 11,033 | 58.1 | 22,066 | 58.1 | 0.000 |
| Female | 7,943 | 41.9 | 15,886 | 41.9 | 0.000 |
| Income level (NTD) | |||||
| Financially dependent | 9,674 | 51.0 | 18,965 | 50.0 | 0.020 |
| 15,840–19,999 | 6,196 | 32.7 | 12,981 | 34.2 | 0.033 |
| 20,000–39,999 | 1,941 | 10.2 | 3,606 | 9.5 | 0.024 |
| 40,000–59,999 | 714 | 3.8 | 1,478 | 3.9 | 0.007 |
| ≥60,000 | 451 | 2.4 | 922 | 2.4 | 0.003 |
| Comorbidities | |||||
| Charlson Comorbidity Index | 1.9 | ±2.1 | 1.1 | ±1.7 | 0.390 |
| Diabetes mellitus | 4,026 | 21.2 | 5,555 | 14.6 | 0.172 |
| Hypertension | 8,564 | 45.1 | 12,776 | 33.7 | 0.236 |
| Thyroid dysfunction | 233 | 1.2 | 293 | 0.8 | 0.046 |
| Depression | 894 | 4.7 | 697 | 1.8 | 0.162 |
| Osteoporosis | 1,070 | 5.6 | 1,107 | 2.9 | 0.135 |
| Medication use | |||||
| Steroids | 1,250 | 6.6 | 1,745 | 4.6 | 0.087 |
| Diuretics | 2,887 | 15.2 | 3,883 | 10.2 | 0.150 |
| Statins | 2,222 | 11.7 | 3,387 | 8.9 | 0.092 |
| PPIs | 1,094 | 5.8 | 1,025 | 2.7 | 0.153 |
| Thyroxine | 185 | 1.0 | 263 | 0.7 | 0.031 |
| Antithyroid drugs | 86 | 0.5 | 121 | 0.3 | 0.021 |
| Hypnotics and sedatives | 2,874 | 15.2 | 2,891 | 7.6 | 0.239 |
| Antiosteoporotic drugs | 290 | 1.5 | 360 | 1.0 | 0.052 |
Continuous variables are reported as means ± standard deviation; categorical variables are reported as numbers and percentages.
Abbreviations: LUTS, lower urinary tract symptoms; NTD, New Taiwan Dollars; PPI, proton pump inhibitor; SMD, standardized mean difference; SD, standard deviation.
Considering certain covariates were disproportionate between the groups, a sensitivity analysis was performed with 1:1 propensity score matching; this was based on the previous constructed study population (by 1:2 age, sex, and index year matching) to balance the baseline differences and evaluate the robustness of the study findings. The propensity score was calculated to estimate the probability of obtaining LUTS diagnosis using logistic regression models based on all covariates listed in Table 1. The analysis was performed using the nearest-neighbor matching algorithm without replacement, employing a caliper width equal to 0.2 times the standard deviation of the logit of the propensity score.
A total of 56,928 patients was enrolled. The LUTS cohort comprised 18,976 subjects; the comparison cohort contained 37,952 patients (Fig 1). Being matched for age, sex, and index year, the proportion of study subjects with comorbidities and specific medication was greater in LUTS than the comparison group. The patient characteristics are displayed in Table 1. The mean follow-up duration was observed as 5.8 years.
During follow-up, 893 and 653 hip fractures were reported in the LUTS and comparison groups, respectively. The Nelson–Aalen estimates in Fig 2 indicated the cumulative risk of hip fracture was greater in the LUTS group (log-rank test, p < 0.001). The incidence of hip fracture was 7.0/1000 and 5.0/1000 person-years in the LUTS and comparison groups, respectively. Univariable and multivariable Cox regression analysis findings are provided in Table 2. Based on univariable analysis, LUTS was significantly associated with an increased hip fracture risk (HR = 1.39, 95% CI: 1.27–1.53, p < 0.001); the connection remained significant in both multivariable analysis models (model 1: aHR = 1.29, 95% CI: 1.17–1.42, p < 0.001; model 2: aHR = 1.30, 95% CI: 1.18–1.43, p < 0.001). Table 3 shows the HR of each covariate for the hip fracture risk in the three Cox regression prototypes and those included in the multivariable model 2.

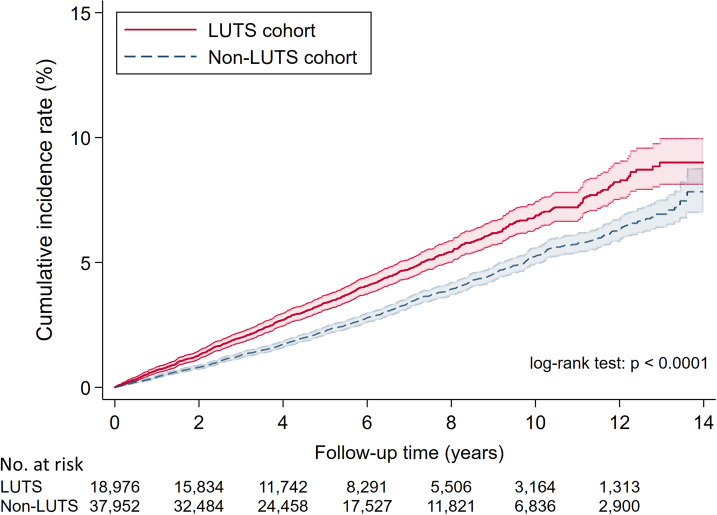
Cumulative incidence curves with 95% confidence intervals (colored zone) of hip fracture in LUTS patients and the comparison group.

| LUTS | ||
| Yes | No | |
| Number of patients | 18,976 | 37,952 |
| Hip fracture events | 772 | 1,156 |
| Person-years | 110,737 | 230,368 |
| Incidence rate* | 7.0 | 5.0 |
| Univariable model | ||
| Crude HR (95% CI) | 1.39 (1.27–1.53) | 1.00 (ref.) |
| P value | <0.001 | |
| Multivariable model 1† | ||
| Adjusted HR (95% CI) | 1.29 (1.17–1.42) | 1.00 (ref.) |
| P value | <0.001 | |
| Multivariable model 2‡ | ||
| Adjusted HR (95% CI) | 1.30 (1.18–1.43) | 1.00 (ref.) |
| p value | <0.001 | |
*Per 1000 person-years
†Multivariable Cox regression model adjusted for all covariates shown in Table 1.
‡Multivariable Cox regression model that applied a forward selection procedure using score test method with p<0.1 as entry-level to include baseline characteristics for adjustment.
Abbreviations: LUTS, lower urinary tract symptoms; HR, hazard ratio; CI, confidence interval; ref., reference.

| Univariable model | Multivariable model 1† | Multivariable model 2‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Crude HR | 95% CI | p value | aHR | 95% CI | p value | aHR | 95% CI | p value | |
| LUTS | 1.39 | 1.27–1.53 | <0.001 | 1.29 | 1.17–1.42 | <0.001 | 1.30 | 1.18–1.43 | <0.001 |
| Age, year | 1.11 | 1.10–1.11 | <0.001 | 1.10 | 1.10–1.11 | <0.001 | 1.10 | 1.10–1.11 | <0.001 |
| Sex | |||||||||
| Male | 1.00 | ref. | 1.00 | ref. | 1.00 | ref. | |||
| Female | 1.46 | 1.34–1.60 | <0.001 | 1.60 | 1.46–1.76 | <0.001 | 1.63 | 1.48–1.78 | <0.001 |
| Income level (NTD) | |||||||||
| Financially dependent | 1.00 | ref. | 1.00 | ref. | 1.00 | ref. | |||
| 15,840–19,999 | 0.80 | 0.73–0.88 | <0.001 | 1.02 | 0.93–1.12 | 0.680 | 1.02 | 0.92–1.12 | 0.722 |
| 20,000–39,999 | 0.25 | 0.19–0.32 | <0.001 | 0.84 | 0.64–1.10 | 0.205 | 0.83 | 0.64–1.09 | 0.191 |
| 40,000–59,999 | 0.15 | 0.09–0.25 | <0.001 | 0.54 | 0.32–0.90 | 0.017 | 0.53 | 0.32–0.89 | 0.016 |
| 60,000 above | 0.08 | 0.04–0.20 | <0.001 | 0.33 | 0.14–0.80 | 0.014 | 0.33 | 0.14–0.80 | 0.014 |
| Comorbidities | |||||||||
| Charlson comorbidity index | 1.20 | 1.18–1.22 | <0.001 | 1.07 | 1.04–1.10 | <0.001 | 1.08 | 1.05–1.11 | <0.001 |
| Diabetes mellitus | 1.83 | 1.64–2.03 | <0.001 | 1.27 | 1.12–1.45 | 0.000 | 1.27 | 1.12–1.45 | 0.000 |
| Hypertension | 1.86 | 1.70–2.03 | <0.001 | 1.06 | 0.96–1.17 | 0.255 | - | - | - |
| Thyroid dysfunction | 0.94 | 0.58–1.54 | 0.814 | 0.76 | 0.40–1.46 | 0.417 | - | - | - |
| Depression | 1.45 | 1.14–1.83 | 0.002 | 1.13 | 0.88–1.44 | 0.349 | - | - | - |
| Osteoporosis | 2.00 | 1.70–2.35 | <0.001 | 1.16 | 0.96–1.40 | 0.116 | - | - | - |
| Medication use | |||||||||
| Steroids | 1.41 | 1.18–1.70 | 0.000 | 1.02 | 0.85–1.23 | 0.818 | - | - | - |
| Diuretics | 1.89 | 1.68–2.13 | <0.001 | 1.05 | 0.92–1.19 | 0.489 | - | - | - |
| Statins | 1.13 | 0.96–1.32 | 0.136 | 0.82 | 0.70–0.97 | 0.020 | 0.83 | 0.71–0.98 | 0.029 |
| PPIs | 1.28 | 1.01–1.64 | 0.043 | 0.94 | 0.73–1.20 | 0.606 | - | - | - |
| Thyroxine | 0.99 | 0.59–1.68 | 0.974 | 1.01 | 0.56–1.82 | 0.970 | - | - | - |
| Antithyroid drugs | 1.28 | 0.64–2.57 | 0.482 | 1.60 | 0.69–3.68 | 0.270 | - | - | - |
| Hypnotics and sedatives | 1.78 | 1.57–2.01 | <0.001 | 1.20 | 1.05–1.38 | 0.007 | 1.24 | 1.09–1.41 | 0.001 |
| Antiosteoporotic drugs | 3.44 | 2.63–4.50 | <0.001 | 1.31 | 0.97–1.77 | 0.079 | 1.46 | 1.11–1.92 | 0.006 |
†Multivariable Cox regression model with adjustment for all covariates listed in Table 1.
‡Multivariable Cox regression model that applied a forward model selection procedure using score test method with p < 0.1 as entry-level to include baseline characteristics for adjustment.
Abbreviations: LUTS, lower urinary tract symptoms; HR, hazard ratio; aHR, adjusted hazard ratio; CI, confidence interval; NTD, New Taiwan dollar.
Univariable and multivariable regression analysis findings after stratification by sex and age are shown in Table 4. After stratification for sex, LUTS was significantly associated with an increased hip fracture risk in both men (aHR = 1.24, 95% CI: 1.08–1.42; p = 0.003) and women (aHR = 1.34, 95% CI: 1.18–1.53; p < 0.001) in multivariable model 1. LUTS increased hip fracture risk in patients aged 65–79 years (aHR = 1.29, 95% CI: 1.14–1.45; p < 0.001) and ≥80 years (aHR = 1.30, 95% CI: 1.07–1.58; p = 0.008). The association between LUTS and increased hip fracture risk in patients aged 50–64 years was not significant (aHR = 1.11, 95% CI:0.87–1.43; p = 0.397). The interaction tests did not find any subgroup effects of sex and age on hip fracture risk (sex, p for interaction = 0.557; age, p for interaction = 0.665).

| Subgroup | Univariable model | Multivariable model 1† | Multivariable model 2‡ | |||||
|---|---|---|---|---|---|---|---|---|
| Crude HR (95% CI) | p value | aHR (95% CI) | p value | p for interaction | aHR (95% CI) | p value | p for interaction | |
| Sex | 0.557 | 0.501 | ||||||
| Male | 1.36 (1.18–1.55) | <0.001 | 1.24 (1.08–1.42) | 0.003 | 1.26 (1.10–1.45) | 0.001 | ||
| Female | 1.43 (1.26–1.62) | <0.001 | 1.34 (1.18–1.53) | <0.001 | 1.35 (1.18–1.53) | <0.001 | ||
| Age (years) | 0.665 | 0.851 | ||||||
| 50–64 | 1.36 (1.07–1.73) | 0.011 | 1.11 (0.87–1.43) | 0.397 | 1.15 (0.90–1.47) | 0.282 | ||
| 65–79 | 1.46 (1.30–1.64) | <0.001 | 1.29 (1.14–1.45) | <0.001 | 1.29 (1.14–1.45) | <0.001 | ||
| ≥80 | 1.37 (1.14–1.65) | 0.001 | 1.30 (1.07–1.58) | 0.008 | 1.34 (1.11–1.62) | 0.003 | ||
Patients without LUTS were the reference group in the Cox proportional hazards regression models.
†Multivariable Cox regression model adjusted for the covariates in Table 1.
‡Multivariable Cox regression model that applied a forward selection procedure using score test method with p < 0.1 as entry-level to include baseline characteristics for adjustment.
Abbreviations: LUTS, lower urinary tract symptoms; HR, hazard ratio; aHR, adjusted hazard ratio; CI, confidence interval.
In the sensitivity analysis with propensity score matching, the patient characteristics were balanced-well with all standardized mean differences < 0.1; this indicated negligible difference between the groups (S1 Table). After propensity score matching, an elevated risk of hip fracture was observed in patients with LUTS. The aHRs in the multivariable models 1 and 2 were 1.19 (95% CI: 1.07–1.33, p = 0.001) and 1.20 (95% CI: 1.08–1.33, p < 0.001), respectively. This indicated the robustness of the study findings (S2 Table).
An association was observed between LUTS and the hip fracture risk which remained after stratification by sex and age. Compared to the subjects in the comparison group, LUTS patients bore a 29% elevated risk of developing fractures.
Previous studies evaluating the association between LUTS and the hip fracture risk in men have reported inconsistent findings [15, 27–30]. In women, a direct link has been reported [31–33]; however, Schluter et al. failed to demonstrate such an association [27]. In the present study, LUTS was associated with the hip fracture risk in both Taiwanese men and women.
A systematic review did not recognize any association between OAB medications and hip fractures [16]; however, a recent study in Korea reported an increase in the fracture risk (HR 2.19 95% CI: 1.74–2.77) with the use of α-blockers by female patients with LUTS [20]. Another investigation reported male patients consuming prostate-specific α-antagonists faced elevated risks of falls and fractures due to induced hypotension, and a third study reported both medications and nocturia increased the hip fracture risk in elderly individuals [29, 34]. In the present study, the association between LUTS and the increased hip fracture risk was unaffected by sex or age; however, the relationship between OAB medication and the risk of falls or fractures is required to be explored.
It is unknown how LUTS impacts hip fractures. There are several possible explanations. In elderly men, moderate or severe LUTS at night may be associated with an increased risk of falls and hip fractures [30, 35]. Moreover, orthostatic hypotension associated with prostate-specific α-antagonists may lead to falls [34]. Hip fractures may occur in elderly patients with both LUTS and osteoporosis. This is independently associated with an increased risk of fracture and the formation of bladder stones [36–38]. Secondary studies are required to investigate the causal relationships of LUTS with hip fractures.
The present study data was extracted from insurance claims covering more than 23 million people in Taiwan. However, the long-term follow-up of adults with LUTS experiencing hip fractures was impossible, therefore, a retrospective cohort study including population data was appropriate. The routine long-term clinical follow-up of patients with LUTS allows for identifying those with ICD-9-CM codes for hip fracture in the insurance database. The large population cohort featuring patients with both LUTS and hip fractures was considered to be representative of adults aged ≥50 years in Taiwan. Likewise, the medical practice patterns would be characteristic of the work-up, diagnosis, and treatment.
The limitations feature the inclusion of the LUTS cohort with comorbidities (diabetes, dementia, and medication use involving hypnotics and sedatives) associated with hip fractures [6, 39, 40]; the adjustment for covariates decreased the influence of comorbidities and medication in the present study. Data related to lifestyle habits (smoking and alcohol consumption), substance abuse, chronic hyperglycemia related to hip fracture, body mass index, physical characteristics, and a history of frailty and falls (potentially related to LUTS) were unavailable [41, 42]. Likewise, the unavailability of bone mineral density data occurred due to the non-retrieval of imaging or detailed medical records. This may cause bias, therefore, the present study findings should be interpreted cautiously.
Dual‐energy X‐ray absorptiometry may have been effective for indicating the etiology of fractures; body mass index (BMI) influences bone mineral density, impacting the risk of fracture [43, 44]. Database anonymity made it impossible to contact patients to confirm diagnoses and outcomes; upcoding may result in issues during analysis [45]. Contact with patients could have helped confirm the clinical status, diagnostic information, hospital admission, surgery, and database records, as well as, improve the accuracy of the study. Insurance data may have resulted in selection bias as greater claims ensue increased chances of LUTS diagnosis. Conversely, in another study, patients had under-reported symptoms to their caregivers, resulting in decreased diagnosis [46]. Lastly, the retrospective design using LHID may have introduced an imbalance of health status between the LUTS and comparison groups; selection bias resulted due to differences not evident from the claims data. The ICD-9-CM coding system may not precisely identify the patients in each group. To avoid miscoding, three successive diagnoses of LUTS were required for eligibility. The database was large, but not ethnically diverse; it may apply only to Taiwan. Population-based geographically and ethnically diverse studies would strengthen the findings.
The study detected an association between LUTS and an increased risk of developing hip fractures. Extensive prospective studies are required to explore whether the association is causative.
| aHR | adjusted hazard ratio |
| CI | confidence interval |
| HR | hazard ratio |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| LHID | Longitudinal Health Insurance Database |
| LUTS | lower urinary tract symptoms |
| MrOS | Osteoporotic Fractures in Men |
| NHI | National Health Insurance |
| NTD | New Taiwan Dollars |
| OAB | overactive bladder |
| OR | odds ratio |
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
42
43
44
45
46