
A Pooled Cohort Analysis
Supplemental Digital Content is available in the text.
The 2017 American College of Cardiology/American Heart Association high blood pressure (BP) guidelines recommend risk assessment of atherosclerotic cardiovascular disease to inform hypertension treatment in adults with elevated BP or low-risk stage I hypertension. The use of coronary artery calcium (CAC) score to guide hypertension therapy has not been adequately evaluated. Participants free of cardiovascular disease were pooled from Multi-Ethnic Study of Atherosclerosis, Coronary Artery Risk Development in Young Adults, and Jackson Heart Study. The risk for incident cardiovascular events (heart failure, stroke, coronary heart disease), by CAC status (CAC-0 or CAC>0) and BP treatment group was assessed using multivariable-adjusted Cox regression. The 10-year number needed to treat to prevent a single cardiovascular event was also estimated. This study included 6461 participants (median age 53 years; 53.3% women; 32.3% Black participants). Over a median follow-up of 8.5 years, 347 incident cardiovascular events occurred. Compared with those with normal BP, the risk of incident cardiovascular event was higher among those with elevated BP/low-risk stage I hypertension and CAC>0 (hazard ratio, 2.4 [95% CI, 1.7–3.4]) and high-risk stage I/stage II hypertension (BP, 140–160/80–100 mm Hg) with CAC>0 (hazard ratio, 2.9 [95% CI, 2.1–4.0]). A similar pattern was evident across racial subgroups and for individual study outcomes. Among those with CAC-0, the 10-year number needed to treat was 160 for elevated BP/low-risk stage I hypertension and 44 for high-risk stage I or stage II hypertension (BP, 140–160/80–100 mm Hg). Among those with CAC>0, the 10-year number needed to treat was 36 and 22, respectively. Utilization of the CAC score may guide the initiation of hypertension therapy and preventive approaches to personalize cardiovascular risk reduction among individuals where the current guidelines do not recommend treatment.
High blood pressure (BP) is associated with an increased risk of adverse cardiovascular events,1–3 and nearly half of the United States population across various age-groups have hypertension as per the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines.1–5 The stratification of patients based on the 10-year risk of adverse cardiovascular events using the ACC/AHA Pooled Cohort Equation has been proposed to guide the treatment of patients with elevated BP or low-risk stage I hypertension.2,6 However, the equation does not accurately predict risk for atherosclerotic cardiovascular disease (ASCVD) in racially diverse cohorts and provides only modest prognostic insight for risk stratification.7–9
The coronary artery calcium (CAC) score is a commonly used cardiac imaging marker that has been previously validated for predicting the risk of adverse cardiovascular events in multiethnic and racially diverse cohorts.10–13 The risk of cardiovascular mortality in hypertensive patients can be effectively assessed using the CAC score.10–13 However, the role of a CAC score of zero (CAC-0) to stratify the overall incident cardiovascular event risk, and specifically incident stroke, incident coronary heart disease (CHD), and incident heart failure (HF) in patients with previously untreated hypertension is not known.14 Furthermore, there are limited data on the role of CAC-0 to risk-stratify hypertensive patients within the racial subgroups.14
We hypothesized that a CAC score of zero improves the adverse cardiovascular event risk stratification among individuals with elevated BP and low-risk stage 1 hypertension as per the 2017 ACC/AHA guidelines. We sought to evaluate the use of a CAC-0 score to evaluate the risk of adverse cardiovascular events in various strata of BP and to inform the appropriate use of BP-lowering medications in a multiethnic and diverse pooled cohort.
The data for this study were obtained from the National Heart, Lung, and Blood Institute BioLINCC Data Repository and is available at https://biolincc.nhlbi.nih.gov/home/.
The participant-level data was pooled from 3 prospective cohort studies: (1) the CARDIA Study (Coronary Artery Risk Development in Young Adults),15 (2) the MESA (Multi-Ethnic Study of Atherosclerosis),16 and (3) the JHS (Jackson Heart Study).17 In brief, the CARDIA study enrolled 5115 Black and White individuals aged 18 to 30 years in 1985 to 1986 across 4 centers which included Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. The MESA is a multiethnic cohort study that enrolled 6814 participants aged 45 to 84 years without any known cardiovascular disease between 2000 and 2002 in 6 United States communities. The JHS is a prospective cohort of 5306 Black (3883 with data available in National Heart, Lung, and Blood Institute BioLINCC) individuals aged >20 years enrolled between 2000 and 2004 from the Jackson, Mississippi, tricounty area. In this study, we included participants from the 3 cohorts who were free of cardiovascular diseases (CHD, stroke, and HF) at baseline and had CAC scores available. We included the data from year 15 of CARDIA, visit 1 of MESA, and visit 2 of the JHS. We excluded individuals <40 years of age since the 10-year ASCVD risk (estimated using pooled cohort equations) is recommended for use in adults ≥40 years of age. Given the objective of the study to assess the role of CAC to inform treatment initiation, we excluded individuals who were on antihypertensive treatment at baseline.
In the CARDIA study, the BP was recorded in the sitting position on the right arm using a Hawksley random-zero sphygmomanometer (WA Balm Co) after 5 minutes of rest. Measurements were repeated thrice at 1-minute intervals and the average of the last 2 readings was averaged. Similarly, in MESA, the BP was recorded in a seated position using Dinamap Pro-100 automated oscillometric sphygmomanometer after at least 5 minutes of rest. Three readings were taken and the average of the last 2 was used. In the JHS cohort, BP was recorded in the right arm in a sitting position using Hawksley random-zero sphygmomanometer after resting for at least 5 minutes. Two readings were recorded 1 minute apart, and the average of the 2 readings was used.
The CAC assessment protocols for participants of CARDIA, MESA, and JHS have been previously described.18–20 In brief, cardiac CT was performed using cardiac-gated electron-beam CT scanners (GE-Imatron C-150XL, GE-Imatron, GE LightSpeed 16 Pro, GE LightSpeed Qxi, and Siemens Volume Zoom) at the respective study sites for the various cohorts. The images were viewed and scored as per standardized protocols using TeraRecon Aquarius Workstation (TeraRecon, Inc, San Mateo, CA).
The patients were classified as per the 2017 ACC/AHA BP treatment guidelines for antihypertensive medication initiation. The 3 broad groups included (1) individuals with normal BP (<120/80 mm Hg); (2) individuals with elevated BP (120–129/<80 mm Hg) or low-risk stage I hypertension (130–139/80–89 mm Hg); and (3) high-risk stage I hypertension (130–139/80–89 mm Hg) or stage II hypertension (≥140/90 mm Hg). The patients in the third group are recommended antihypertensive therapy under the current ACC/AHA guidelines. Based on the 2017 ACC/AHA guidelines, high-risk stage I hypertension was defined by additional features alongside BP cutoffs, which included any of the following: age ≥65 years with systolic BP ≥130 mm Hg, diabetes mellitus, 10-year ASCVD risk ≥10% (estimated using pooled cohort equations), and having chronic kidney disease or estimated glomerular filtration rate <60 mL/(min·1.72 m2). The pooled cohort equation for non-Hispanic White individuals was used to compute the 10-year ASCVD risk in participants identifying as White, Hispanic, and Chinese Americans. For this study, besides the abovementioned treatment classification, the patients were further divided based on the presence of a CAC score of zero. The management of patients with BP ≥160/100 mm Hg and those with normal BP is generally consistent across the multiple guideline recommendations, so they were not further stratified on the basis of CAC-0.21–23 The patients were classified into 6 overall groups: (1) normal BP; (2) elevated BP or low-risk stage I hypertension with CAC-0; (3) elevated BP or low-risk stage I hypertension with CAC>0; (4) high-risk stage I hypertension or stage II hypertension with BP <160/10 mm Hg and CAC-0; (5) high-risk stage I hypertension or stage II hypertension with BP <160/10 mm Hg and with CAC>0; (6) stage II hypertension with BP ≥160/100 mm Hg (Figure S1 in the Data Supplement). In sensitivity analysis for the primary outcome, we further stratified CAC score into the subgroups of CAC-0, CAC score 1 to 100, 100 to 400, and ≥400. In the additional sensitivity analysis, we further stratified those with normal BP into those with CAC-0 and CAC>0 (Figure S2).
The primary study outcome was a composite of the first occurrence of CHD (myocardial infarction, revascularization, or resuscitated cardiac arrest due to cardiac causes), stroke, or HF. The secondary outcomes of interest were the individual outcomes of incident CHD, incident stroke, and incident HF. Expert panels in the respective cohorts adjudicated the individual study outcomes as described previously.24–27 The adjudication measures are detailed in Data Supplement.24–37
The individual-level data were pooled, and the participants were categorized into the abovementioned groups. The baseline characteristics were summarized and compared using descriptive statistics. In brief, the continuous variables were summarized as the median and interquartile range and compared using the Kruskal-Wallis test. Categorical data were summarized as counts and percentages and compared using the χ2 test. Kaplan-Meier analyses were used to depict the cumulative incidence of the study outcomes stratified by antihypertensive therapy recommendation and CAC score and compared using the log-rank test. The follow-up time was censored at ten years since the ASCVD risk score estimated using the pooled cohorts equation predicts the risk of ASCVD till up to 10 years. Multivariable-adjusted Cox regression models were used to assess the risk of the study outcomes across the various BP-CAC–based study groups, taking those with normal BP as the reference group. In the sensitivity analysis, we computed the risk of the primary and secondary study outcomes, taking those with normal BP and CAC-0 as the reference group. The analyses were repeated in the race-stratified subgroups. The covariates in the model include age, sex, race, body mass index, smoking status, diabetes, total cholesterol, statin use, high-density lipoprotein-cholesterol, study cohort, and chronic kidney disease. The interaction of race with the CAC-BP groups on the study outcomes was assessed using a multiplicative interaction term. The incidence rates across the various BP-CAC–based study groups in the overall population and across racial subgroups were computed using Poisson regression models. The time-dependent area under the curve was computed for (1) CAC-0 only; (2) 2017 ACC/AHA guidelines based study groups; and (3) CAC-BP–based study groups; as each one predicted the risk of the primary outcome. The Uno’s concordance statistic was computed to assess the change in risk prediction ability of the abovementioned 3 models. We also computed 10-year number needed to treat (NNT10) to prevent the primary and secondary study outcomes in the overall population and in racial subgroups. The NNT10 was computed assuming a 38% relative risk reduction in incident HF, 19% reduction in stroke, 17% reduction in CHD, and 25% relative risk reduction in the primary study outcomes based on the treatment effect of intensive BP control seen in the SPRINT trial (Systolic Blood Pressure Intervention Trial).1,6 Due to substantially smaller population counts and the relatively shorter follow-up periods in the Chinese Americans and Hispanics, we did not compute NNT10 in this population. Based on prior data,13 we performed sensitivity analyses stratifying the population group by CAC score of 220. All statistical analyses were performed using SAS 9.4 (Cary, NC). All tests were 2-sided with a significance level of 0.05.
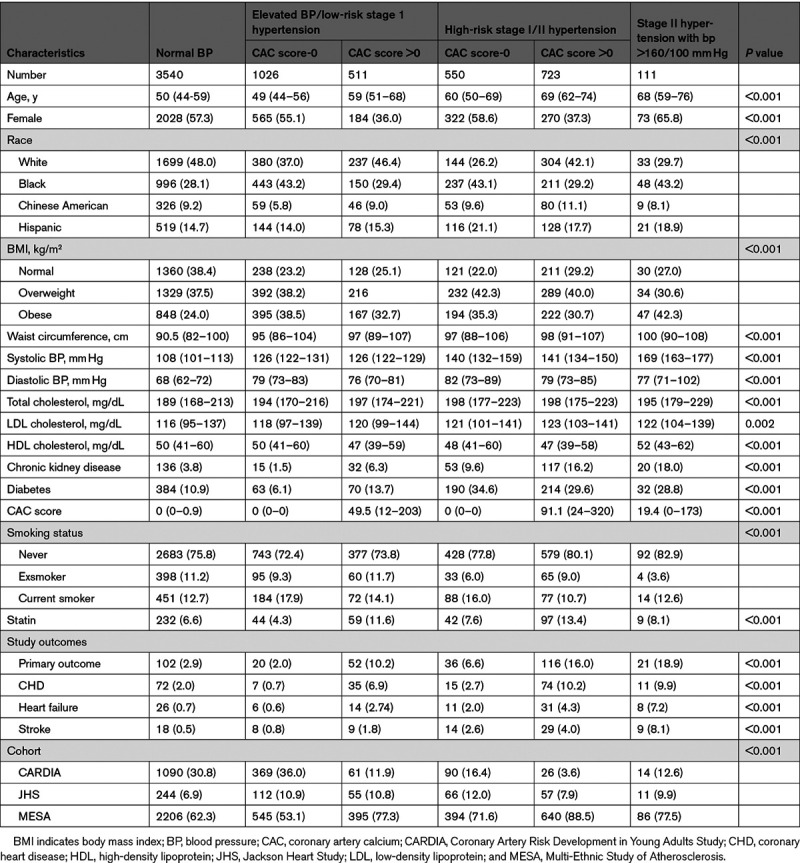
We identified 6461 individuals free of incident cardiovascular disease. The median age was 53 (interquartile range: 45–64) years, and the study population was composed of 53.3% females, 32.3% Blacks, 15.6% Hispanics, and 8.9% Chinese American individuals. Of them, ≈66.0% (4262) had a CAC score of zero. CARDIA, JHS, and MESA contributed 25.6%, 8.4%, and 66.0% of the study population, respectively. In our study, 54.8% had normal BP, 23.8% had elevated BP or low-risk stage I hypertension, 19.7% had high-risk stage I/ hypertension stage II with BP <160/100 mm Hg, and 1.7% had hypertension stage II with BP ≥160/100 mm Hg (Table 1). The baseline patient characteristics of the study population stratified by the 2017 ACC/AHA high BP guideline-recommended treatment groups and CAC-0 status are described in Table 1. Participants with higher BP and those who were recommended antihypertensive therapy were relatively older, with a higher proportion of Blacks, Chinese Americans, and Hispanics, and had a higher prevalence of diabetes and obesity and worse renal function (Table 1). The baseline participant characteristics of the study population with additional CAC-based stratification of those with normal BP is described in Table S1.

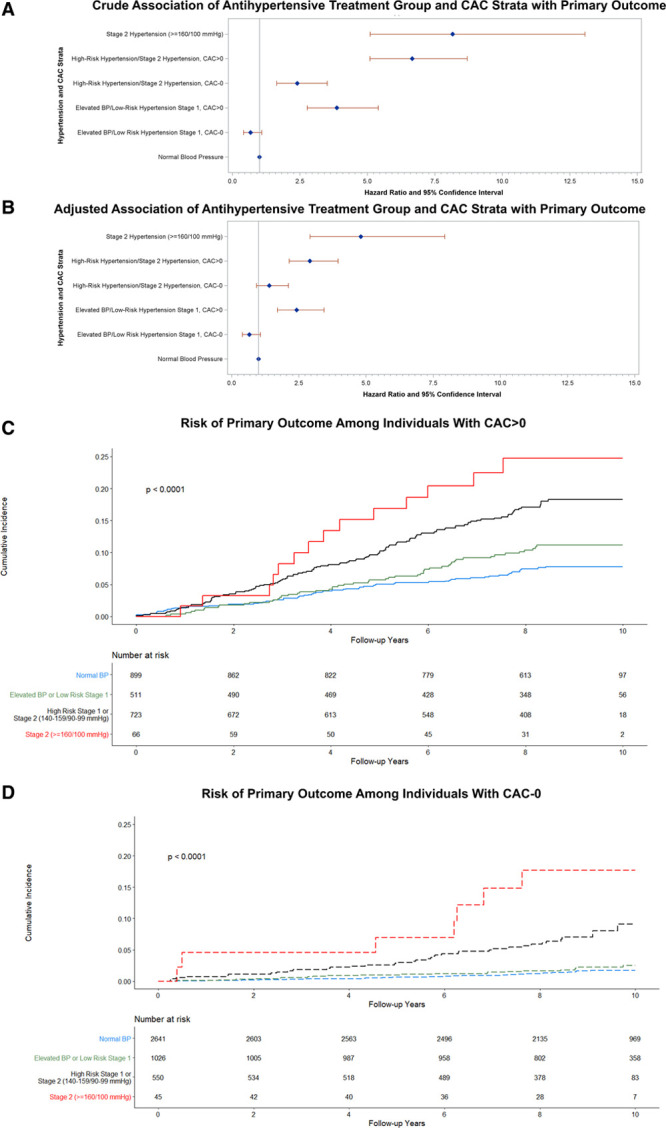
In our study population, there were 347 primary outcome events over a median follow-up period of 8.5 (interquartile range, 7.8–9.3) years. The event rate (per 1000 person-years) for all study outcomes is described in Table 2. In multivariable-adjusted models, taking those with normal BP as the reference, the hazards for the incident adverse cardiovascular event was 0.66 (95% CI, 0.40–1.08) and 2.42 (95% CI, 1.70–3.44) in those with elevated BP/low-risk stage I hypertension, with CAC-0 and CAC>0, respectively. Similarly, taking those with normal BP group as the reference, the hazards for incident adverse cardiovascular event were 1.40 (95% CI, 0.93–2.11) and 2.91 (95% CI, 2.14–3.96) among those with high-risk stage I hypertension or stage II hypertension with BP <160/100 mm Hg, with CAC-0 and CAC>0, respectively (Figure 1). The cohort stratified results for the primary outcome are presented in Table S3. The study outcomes were similar across racial subgroups (Figure 2, Table S4). There was no significant interaction of race and the CAC- and BP-based risk stratification of the study outcomes (P>0.10). The time-dependent area under the curve curves for the prediction of risk of an incident cardiovascular event using classes of BP alone, CAC score alone, and CAC and high BP class combined are depicted in Figure S3. The Uno’s concordance statistic demonstrates that the combination of BP treatment classes with CAC-0 results in a significant improvement in the risk prediction for an incident cardiovascular event (P<0.001) than BP treatment classes or CAC-0 alone. Table S5 depicts the unadjusted and adjusted hazards for the primary outcome when those with CAC>0 were further stratified.

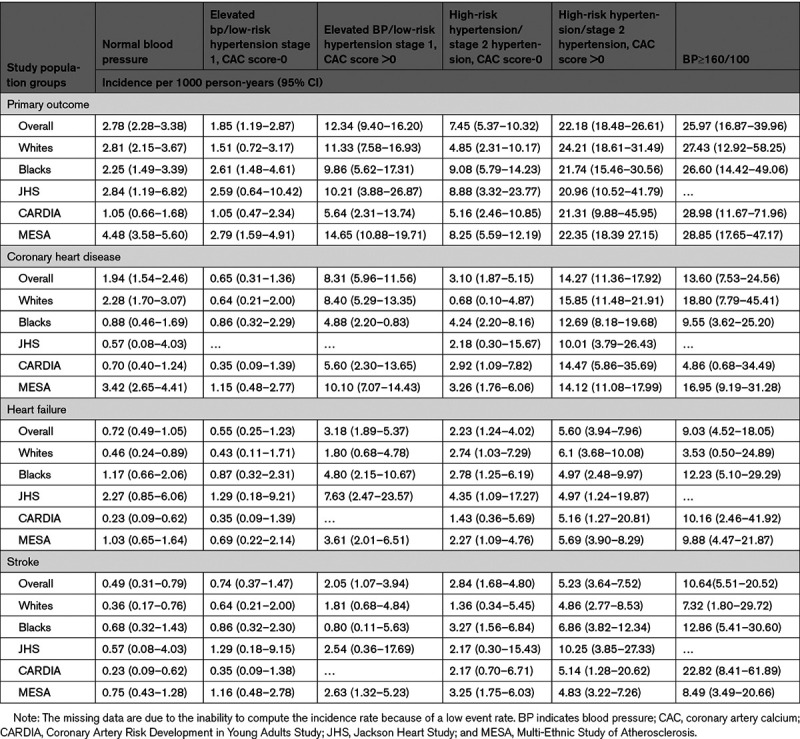

Risk of adverse cardiovascular events: stratified by antihypertensive treatment group and coronary artery calcium (CAC) score. A and B, Forest plots of crude and multivariable-adjusted hazard ratio (blue diamond) with the 95% CI (red error bars). C and D, Kaplan-Meier curves for the risk of cardiovascular events stratified by CAC score. The P values in the Kaplan-Meier Curves represent the log-rank test. BP indicates blood pressure.

Race-stratified risk of adverse cardiovascular events by antihypertensive treatment group and coronary artery calcium (CAC) score. A and B, Kaplan-Meier curves for the risk of cardiovascular events stratified by CAC score among White individuals. C and D, Kaplan-Meier curves for the risk of cardiovascular events stratified by CAC among Black individuals. The P values in the Kaplan-Meier Curves represent the log-rank test. BP indicates blood pressure.
In our sensitivity analysis, taking those with normal BP and CAC-0 as the reference, the risk of the primary outcome was higher in those with normal BP and CAC>0 (hazard ratio [HR], 3.41 [95% CI, 2.23–5.23]), elevated BP/low-risk stage I hypertension and CAC>0 (HR, 4.74 [95% CI, 3.04–7.41]), high-risk stage I hypertension/stage II hypertension (BP<160/100 mm Hg) and CAC-0 (HR, 2.69 [95% CI, 1.65–4.40]), and high-risk stage I hypertension/stage II hypertension (BP<160/100 mm Hg) and CAC>0 (HR, 6.05 [3.96–9.24]), and stage II hypertension with BP≥160/100 mm Hg (HR, 9.47 [95% CI, 5.35–16.76]; Table S6, Figure S4). The incidence rate for all study outcomes for this sensitivity analysis is depicted in Table S7.
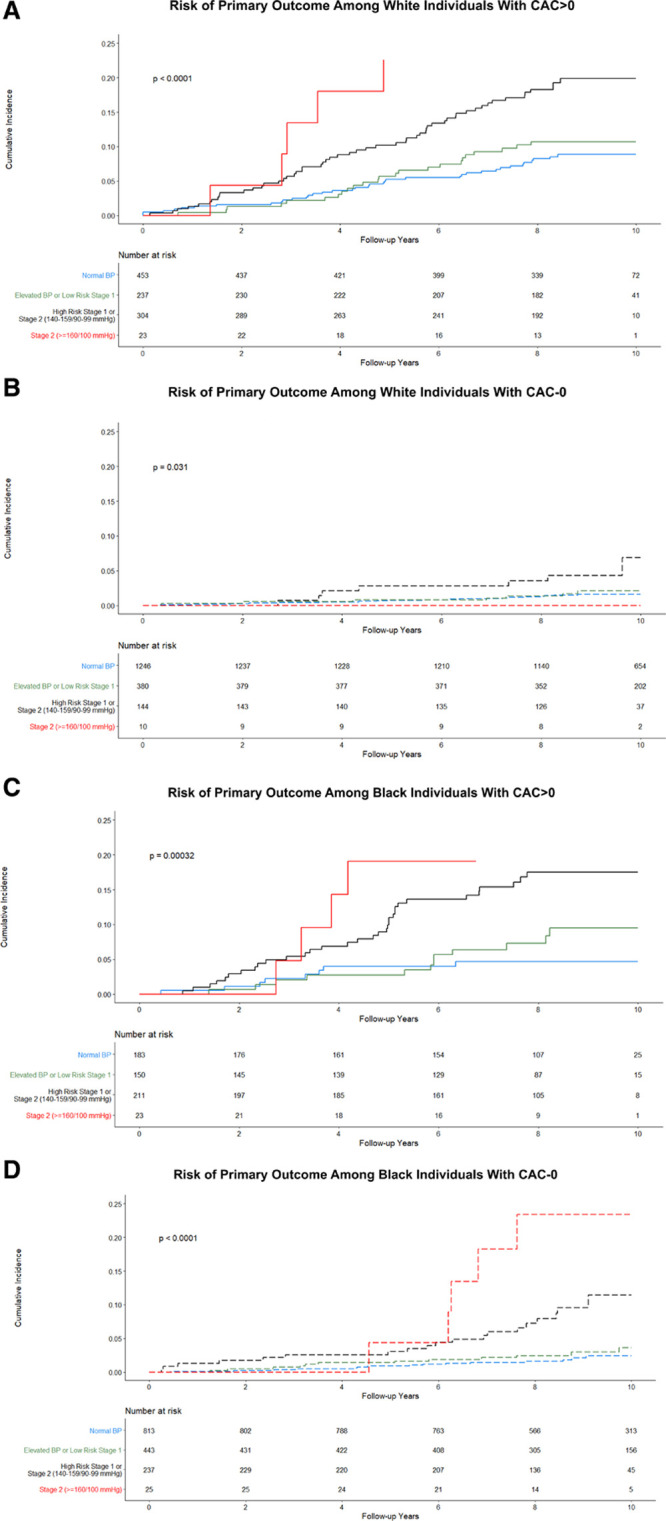
In our study cohorts, there were 96 HF events, 87 stroke events, and 214 CHD events. Controlling for covariates and taking those with normal BP as a reference, the risk of CHD was higher for those with elevated BP/low-risk stage I hypertension with CAC>0 (HR, 2.36 [95% CI, 1.55–3.60]), those with high-risk stage I hypertension/stage II hypertension (BP <160/100 mm Hg) and with CAC>0 (HR, 2.64 [95% CI, 1.81–3.83]), and stage II hypertension with BP >160/100 mm Hg (HR, 3.70 [95% CI, 1.89–7.25]; Figure 3, Figure S5 through S7). Those with elevated BP/low-risk stage I hypertension with CAC-0 had a lower risk of CHD (HR, 0.36 [95% CI, 0.17–0.79]) compared with those with normal BP. The risk of incident HF, compared with those having normal BP, was higher in individuals with CAC>0 and having low-risk elevated BP/stage I hypertension (HR, 2.15 [95% CI, 1.07–4.28]), those with high-risk stage I hypertension/stage II hypertension with BP <160/100 mm Hg and CAC>0 (HR, 2.15 [95% CI, 1.20–3.83]), and stage II hypertension with BP >160/100 mm Hg (HR, 3.90 [95% CI, 1.66–9.13]). The risk of incident stroke was higher in all BP treatment groups apart from those with CAC-0 and elevated BP/low-risk stage I hypertension (P<0.05 for all). The race-stratified results for the HF, stroke, CHD outcomes are presented in Table S4. The incidence rate for the study outcomes across the BP and CAC-0 strata overall, in the racial subgroups, and by cohorts are depicted in Table 2.

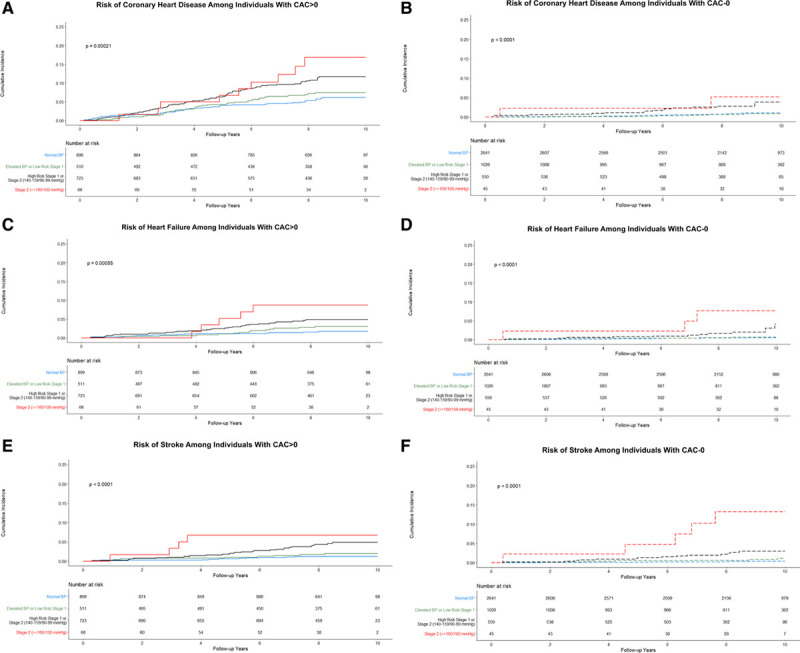
Kaplan-Meir curves for the risk of study outcomes by antihypertensive treatment group and coronary artery calcium (CAC) score. The figure represents the Kaplan-Meier curves for the risk of coronary heart disease (A and B), heart failure (C and D), and stroke outcome (E and F) stratified by CAC score. The P values in the Kaplan-Meier Curves represent the log-rank test. BP indicates blood pressure.
In the sensitivity analysis, taking those with normal BP and CAC-0 as a reference, individuals with normal BP and CAC>0, elevated BP/low-risk stage I hypertension and CAC-0 or CAC>0, high-risk stage I hypertension/stage II hypertension (BP<160/100 mm Hg) and CAC=0 or CAC>0, and those with stage II hypertension and BP ≥160/100 mm Hg had a higher risk of all secondary outcomes (Figure S8 through S10, Table S6). The results of the sensitivity analyses using CAC score of 220 as cutoff are depicted in Table S8.
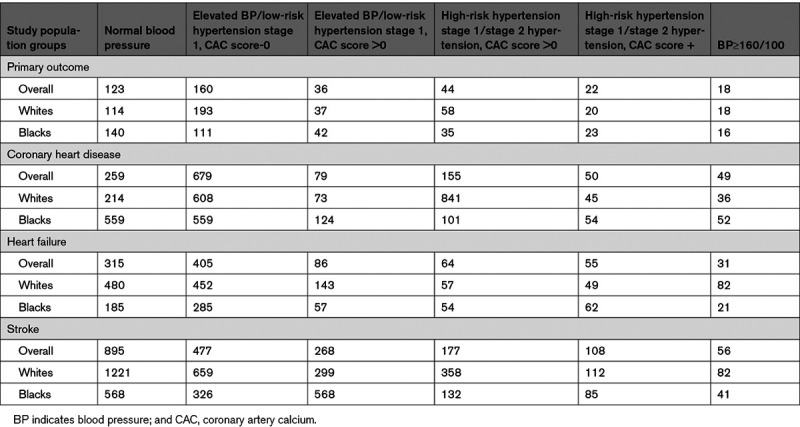
Among patients with elevated BP/low-risk stage I hypertension (not recommended medication), the NNT10 for prevention of one incident adverse cardiovascular event was 160 and 36 in participants with CAC-0 and CAC>0, respectively. Among patients with high-risk stage I hypertension/stage II hypertension with BP <160/100 mm Hg, the NNT10 for prevention of incident adverse cardiovascular events was 44 and 22 in participants with CAC-0 and CAC>0, respectively. The NNT10 for the primary outcome was 18 in those with BP ≥160/100 mm Hg. For White participants with elevated BP/low-risk stage I hypertension, the NNT10 for preventing incident cardiovascular events was 193 and 37 in participants with CAC-0 and CAC>0, respectively. For Black participants with elevated BP/low-risk stage I hypertension, the NNT10 was 111 and 42. The NNT10 for prevention of incident adverse cardiovascular events in White participants with high-risk stage I hypertension/stage II hypertension with BP <160/100 mm Hg was 58 and 20 in those with CAC-0 and CAC>0, respectively. In Black participants, the NNT10 for preventing incident cardiovascular event in those with stage I hypertension/stage II hypertension with BP <160/100 mm Hg was 35 and 23 in those with CAC-0 and CAC>0, respectively. The NNT10 for preventing CHD, HF, and stroke across the various BP groups overall and among racial subgroups are depicted in Table 3.

In this pooled cohort study encompassing >6000 individuals, we observed significant heterogeneity in the incident cardiovascular risk captured by CAC score across different strata of BP. We observed that nearly a third of individuals with elevated BP or low-risk stage I hypertension who are not recommended initiation of antihypertensive therapy as per the 2017 ACC/AHA guidelines have a CAC>0, which corresponds to a higher risk of incident cardiovascular events compared with those having normal BP. Nearly half of the individuals with high-risk stage I hypertension or with stage II hypertension have CAC-0. The presence of CAC was predictive of an increased risk of adverse cardiovascular events across population treatment groups and identified individuals who may benefit from antihypertensive therapy or being treated to intensive BP goal. Refining risk assessment with the CAC score across BP groups also predicted the risk of incident HF, stroke, and coronary heart disease. The risk prediction ability of CAC-0 for guiding antihypertensive therapy is retained across racial subgroups. CAC-0 was independently associated with a lower risk of adverse cardiovascular events, even among those with normal BP. Cumulatively, the study findings suggest that the use of CAC scores, when available, can assist with personalizing the initiation of antihypertensive therapy in individuals with elevated BP or low-risk stage 1 hypertension.
Prior investigations have assessed the role of CAC score for risk assessment in hypertensive individuals.13,14 Previously, Uddin et al13 identified high-risk patient populations comparable to the SPRINT trial using a CAC score cutoff of 220 who may be candidates for aggressive BP control strategy.14 The prevalence of CAC>0 has been found to increase with higher BP levels even among young, low-risk individuals.38 The utility of CAC scores in a population with elevated BP or low-risk stage 1 hypertension to identify those in the intermediate phenotype having a higher risk of incident adverse cardiovascular event, stroke, coronary heart disease, and HF are not known.39 McEvoy et al40 previously assessed the utility of CAC score in those with hypertension as per the Joint National Committee-8 guidelines. However, a clinically aligned contemporary understanding of CAC score in guiding antihypertensive therapy in light of the SPRINT trial and the 2017 ACC/AHA recommendations across diverse racial groups is not known. Racial/ethnic differences in the prevalence and the prognostic ability of CAC scores have been previously reported.11,41 Although these studies investigated the independent predictive ability of CAC scores in the general population, the risk refinement performance of CAC score in the racial subgroups to guide the initiation of antihypertensive therapy are not known.11,12,42 Our study findings suggest that although racial/ethnic minorities are at a higher risk of adverse cardiovascular events, the risk refinement for the initiation of antihypertensive therapy guided by CAC score has prognostic utility across racial subgroups. In our study of American cohorts, we observed that nearly a third of those not currently recommended treatment have an elevated CAC score (CAC>0). Assuming a similar proportion at a national level, nearly 7.1 million adults from 21.4 million43 not currently recommended treatment would be eligible for antihypertensive therapy. Our study found that CAC-0 may be a tool to guide shared patient-physician decision-making in providing a personalized approach to risk reduction in patients with elevated BP or hypertension, especially those who are not recommended treatment under the current ACC/AHA guidelines. The personalized risk reduction in those with CAC>0 may include a comprehensive approach including antihypertensive therapy, lipid-lowering therapy, and glycemic control, healthy diet, physical activity, and smoking cessation.
The NNT10 for treatment among those with CAC>0 who are currently not recommended antihypertensive therapy under the ACC/AHA guidelines was relatively low. This indicates that a substantial risk reduction may be achieved if these individuals are initiated on pharmacotherapy and undergo intensive BP treatment. Several risk reduction approaches may be used alongside pharmacotherapy that may provide a comprehensive cardiovascular risk reduction in patients with elevated CAC scores who are otherwise deemed to be at a low-risk based on traditional risk factors.27 The comparable NNT10 of those with an elevated CAC in the elevated BP or hypertension across racial groups highlights the plausible efficacy of global use of CAC score to identify the ideal candidates for intensive BP control. Many patients with high-risk stage I hypertension or stage II hypertension with BP <160/100 mm Hg had CAC-0. Although the underlying cardiovascular risk is not obfuscated by CAC-0 in these otherwise high-risk individuals, there may be an advantage in utilizing this clinical information for therapeutic decisions. Before the SPRINT trial, hypertension guidelines had used a higher therapeutic cutoff for elderly individuals, recognizing the limited evidence of aggressive BP control in older individuals.1 Although there may be a small subset of elderly patients with CAC-0, clinicians may consider not escalating antihypertensive therapy among those who cannot tolerate higher BP-lowering doses, such as older individuals with orthostatic hypotension. Furthermore, optimizing BP treatment in patients already on antihypertension therapies should be addressed in future work.
We also observed that those with a CAC-0 and elevated BP/low-risk stage I hypertension had a lower risk of CHD than those with normal BP and CAC >0. Furthermore, CAC>0 is independently predictive of increased adverse cardiovascular risk, even among those with normal BP. This indicates that the CAC score captures underlying subclinical cardiovascular pathological changes, even in the setting of relatively lower cardiovascular risk. This subclinical disease may be captured by CAC>0, despite normal BP levels. The CAC-0 based risk stratification may, therefore, have utility in the primordial prevention of a broad complex of cardiovascular risk factors beyond a single risk factor, such as BP only.44 Since CAC>0 captures an overall risk of ASCVD and other preventive therapies like statins may find utility in this population. There exists a prevention paradox wherein a reasonable proportion of individuals developing cardiovascular events are at a lower predicted risk of cardiovascular disease, and large scale preventive efforts are not targeted towards this group.45,46 Although ascertainment of normal BP may be difficult, the findings from this study and prior investigations44,47 suggest that even those with normal BP may have a relatively high cardiovascular event risk. Hence, CAC-0 may have a role in primary cardiovascular prevention by identifying patients with normal BP in whom intensification of preventive approaches, such as lipid-lowering therapy, glycemic control, healthy diet, physical activity, and smoking cessation should be targeted. The role of the CAC score in primary prevention of cardiovascular disease is an active area of interest,48,49 with recent data indicating elevated CAC score being associated with an increased risk of incident hypertension.50
There are several public health implications of our study. The CAC score is increasingly being integrated into the control of traditional cardiovascular risk factors, such as dyslipidemia.51 Consequently, the CAC score may be available for many primary care patients. Given the estimated additional ≈30 million individuals identified with hypertension by the 2017 ACC/AHA guidelines, the supplementation of the guideline-recommended treatment with the CAC score-driven approach may help in identifying those at the highest cardiovascular risk. This approach, in conjunction with other approaches such as blood biomarker-based strategy (N-terminal-pro-B-type natriuretic peptides and cardiac troponin)6,52 or use of other imaging markers (carotid ultrasound) may help amplify absolute cardiovascular risk reduction through personalized antihypertensive therapy.49 Further investigation is needed to compare the incremental benefit of CAC score–guided and biomarker-guided antihypertensive therapies. CAC-based therapeutic risk stratification is an established, cost-effective approach to reduce adverse cardiovascular event risk.53 Similarly, intensive BP control is a cost-effective risk reduction approach.54 Combining the CAC score–guided cardiovascular risk reduction and intensive BP control, especially in those at a presumed low cardiovascular risk and no pharmacotherapy recommendation under the current guidelines, may prove to be a cost-effective approach. The advantage of cardiovascular risk reduction through control of BP has been established across various patient substrates.47 However, the CAC score may inform the shared patient-physician therapeutic decision-making process in situations where there are limitations to aggressive antihypertensive treatment.49 There may also be clinical utility in the use of CAC score in the assessment of residual cardiovascular risk in patients adequately treated as per the ACC/AHA guidelines. This must be balanced against the risks associated with radiation exposure in the context of universal CAC screening among those with elevated BP or stage I hypertension.55 Also, this study does not advocate for universal CAC score–based screening of patients but rather use this important imaging biomarker when available.
Our study has several limitations. There are inherent differences in the composition and characteristics of the cohorts as the participants were recruited in different regions across the United States. To account for these differences, we included the respective cohort as an adjustment covariate in our analyses. There were also temporal and procedural variations in the assessment of BP across the 3 cohorts. However, all cohorts recorded multiple BP readings in a sitting position, and we included the average of multiple measurements in our analysis. Although we used multivariable-adjusted models in our analyses, residual confounding due to unmeasured confounders (such as BP measurement instruments) cannot be ruled out due to observational study design. The NNT10 was estimated in patients who were stratified according to the current guidelines. The study cohorts were initiated before the introduction of the current guidelines and there may not have been an incentive for intensification of antihypertensive therapy among participants during the follow-up period. Lastly, our findings may need verification in the setting of a randomized clinical trial to assess the efficacy of CAC score–guided management of hypertension compared with the current guideline-based practice.49 Prospective investigations are needed to assess the benefits, costs, and potential harms of CAC scans for a CAC score–based approach to guide hypertension management.
The CAC score is an effective tool to identify individuals across racial subgroups with elevated BP or low-risk stage I hypertension who are at a higher risk of incident CHD, stroke, HF, and adverse cardiovascular events and may benefit from antihypertensive pharmacotherapy. Refinement of risk assessment using the CAC score may help identify additional candidates who may benefit from antihypertensive therapy.
We thank the participants of the CARDIA (Coronary Artery Risk Development in Young Adults), MESA (Multi-Ethnic Study of Atherosclerosis), and JHS (Jackson Heart Study) Studies. We would like to thank the respective cohort investigators for making the data publically available through National Heart, Lung, and Blood Institute (NHLBI) BioLINCC.
This work was supported by the National Institutes of Health Mentored Patient-Oriented Research Award (5K23HL146887-02) to Dr Arora.
None.
| ACC/AHA | American College of Cardiology/American Heart Association |
| ASCVD | atherosclerotic cardiovascular disease |
| BP | blood pressure |
| CAC | coronary artery calcium |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CHD | coronary heart disease |
| HF | heart failure |
| HR | hazard ratio |
| JHS | Jackson Heart Study |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| NNT10 | 10-year number needed to treat |
| SPRINT | Systolic Blood Pressure Intervention Trial |
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
Nearly a third of individuals with elevated blood pressure or low-risk stage I hypertension, who are not recommended treatment as per 2017 American College of Cardiology/American Heart Association high blood pressure Guidelines, have an elevated coronary artery calcium score, which translates to a higher risk of adverse cardiovascular events.
Those with elevated blood pressure/low-risk stage I hypertension and coronary artery calcium >0 have a high-risk of incident coronary heart disease, incident heart failure, and incident stroke.
The increased adverse cardiovascular risk associated with coronary artery calcium>0 was consistent in both White and Black individuals.
In the pooled cohort of over 6000 participants, coronary artery calcium >0 was independently predictive of increased adverse cardiovascular event risk across 2017 American College of Cardiology/American Heart Association hypertension guideline treatment groups and identifies individuals who may benefit from antihypertensive therapy or intensive blood pressure control alongside comprehensive cardiovascular risk reduction approaches.